Ear acupuncture and neuromodulation: narrative review
Introduction
Ear acupuncture is a therapeutic approach that has its own diagnosis and treatment, using cartographies of acupoints distributed on the external surface of the ear; it integrates ancient theoretical-philosophical and current neuroscientific references for the management of somatic, visceral and emotional disorders (1).
The use of the auricular pavilion therapeutically by different antique peoples has been reported, like in China, where its use was based on the theories of Traditional Chinese Medicine, such as the theory of yin-yang channels and their connection with organs (Zang: Liver, Heart, Spleen, Lung and Kidney) and viscera (Fu: Gallbladder, Small Intestine, Stomach, Large Intestine and Bladder), explaining its effects on the body. The Egyptians used ear stimulation as a contraceptive method; while in Greece, the auricular phlebotomy technique was used by Hippocrates to treat men with impotence and infertility (2,3).
In modern age, the Portuguese physician Zacatus Lusitanus described in 1637 the use of this method to treat people with sciatica, and in 1717, the famous Italian physician Antonio Maria Valsalva, known for the Valsalva Maneuver, recorded the use of ear cauterization for of dental pain treatment (1,2). These reports possibly served as a basis for some practitioners to use this type of intervention, which years later contributed to its development (2).
Nowadays, auricular acupuncture is a therapeutic resource that has been growing in popularity and has been institutionalized in national health care systems, including in Brazil through the National Policy for Integrative and Complementary Practices in the Unified Health System (4), as it is considered a cheap, simple, safe and effective treatment recommended for the management of pain and associated disorders (5-8).
In this regard, acquiring knowledge of its neuromodulatory mechanisms and effects is of utmost importance to support its clinical practice and guide professionals in choosing the most appropriate methods and regions for auricular stimulation. This narrative review aims to describe the evolution of auricular acupuncture and its effects on neuromodulation of pain and other disorders. Its relevance stands out in realizing a state of the art that transits between traditional foundations of auricular acupuncture and its biological plausibility.
We present the following article in accordance with the Narrative Review reporting checklist (available at https://lcm.amegroups.com/article/view/10.21037/lcm-21-42/rc).
Methods
This narrative review began with a literature search using the PubMed/MEDLINE database, without restrictions regarding the year, for articles written only in English language including: Auricular Acupuncture OR Auriculotherapy AND Pain AND Neuromodulation OR Auricular Vagus Nerve Stimulation. A multidisciplinary group of researchers searched, reviewed and interpreted preclinical and clinical studies, as well as review studies. Searches were conducted until June and an update was performed in October 2021. Over 123 studies were found and 38 were included in this review. The articles were chosen according to their relevance to the purpose of the review based on the authors’ clinical and research experience in acupuncture and auriculotherapy. Our search strategy summary is illustrated in Table 1.
Table 1
| Items | Specification |
|---|---|
| Date of search | June 2021 and an update in January 2022 |
| Databases and other sources searched | PubMed/MEDLINE |
| Search terms used | Auricular Acupuncture OR Auriculotherapy AND Pain AND Neuromodulation OR Auricular Vagus Nerve Stimulation |
| Timeframe | Without restrictions |
| Inclusion criteria | Only in English language |
| Selection process | A multidisciplinary group of researchers searched, reviewed and interpreted preclinical and clinical studies, as well as review studies, conducted non-independently |
Auricular cartography
The Yellow Emperor’s Classic Book of Internal Medicine, composed as a dialogue between the emperor and his ministers of health, has several texts on the practice of acupuncture (9). It is believed that these texts are probably a collective work of many practitioners that was compiled over many centuries, representing a compendium of medical knowledge accumulated in ancient China over 4,000 years. According to this text, there were reactive acupuncture points on the ear that were sensitive to palpation and were called “Yang Alarm” points, which indicated a pathological disorder of excess Yang. However, the ancient Chinese ear acupuncture charts have no logical order or anatomical basis. Some Chinese texts such as Prescriptions for Emergencies (281 BCE) and Thousand Gold Remedies (581 BCE), traced ear acupuncture treatments for different diseases (10), as jaundice and a variety of epidemics. The Compendium of Acupuncture and Moxibustion [1602] recorded moxibustion on the ear apex point to treat cataracts and described the use of hands to pull down the ear lobes to cure headaches (11).
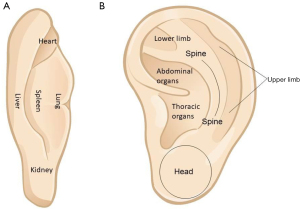
Although auricular stimulation for therapeutic purposes has been mentioned since before Christ, the first document that divided the auricular pavilion into regions representing distant parts of the human body dates back to 1888, where Zhang Di-Shan described the location of the heart, lung, liver, spleen, and kidney represented on the central and peripheral regions of the auricular dorsum (Figure 1) (3,12). The first auricular cartography showing somatic and visceral structures together organized in a homuncular form on the auricle was proposed at the end of the 1950s by the French physician Paul Nogier. He developed a new method of diagnosis and treatment from the auricle called auriculotherapy (13). At the time, his patients reported a treatment for sciatica by cauterization of a specific region of the ear, a practice that was performed by “healers” in the Corsica region of France. It was from this observation that Nogier began his clinical experiments, based on trial and error, in the search for sensitive points on the surface of the ear in response to various clinical conditions of his patients. Based on his observations, Nogier developed an inverted representation of the human body on the auricle, where the musculoskeletal structures were represented on the outer parts of the auricle and the visceral organs on the central shell (Figure 1) (3).
Nogier’s work was presented at conferences and published in a German acupuncture journal of the time (1). His publication served as an impetus for the development of auricular therapy in China, where it is called auricular acupuncture. In the late 1950s, the Nanjing army team of researchers began a clinical trial with more than 2,000 patients to evaluate the method developed by Nogier. From that moment on, auricular acupuncture gained popularity in China. Many auricular maps with different nomenclatures and point locations were developed, which showed the need to standardize the Chinese method. Thus, the first cartographic standardization of ear acupuncture in China occurred in the late 1970s (2,13-15).
Possibly the first attempt at scientific validation of ear charting was in 1980, when researcher Oleson published in the journal Pain a double-blind study that verified the diagnostic accuracy of points on the auricle that represented the musculoskeletal system. Oleson used 40 volunteers with complaints of musculoskeletal pain who were evaluated first by an orthopedist and later by a professional trained in auricular diagnosis. The agreement between medical and auricular diagnosis was 75%, considered statistically significant, demonstrating the presence of somatotopic organization on the auricular pavilion corresponding to the places where the volunteers suffered their somatic complaints (16).
Proving the existence of points on the ear that represent different parts of the body has always been a great challenge for science. In 2002, the Italian physician and researcher David Alimi conducted an experiment that showed, by means of functional magnetic resonance imaging (fMRI), the same activation of the somatosensory cortex S1 by stimulation when pressing the thumb of one hand on a volunteer, as well as by mechanical stimulation on the ear region representing the thumb, according to the map proposed by Nogier (17). Years later, Marcos Romoli, also an Italian physician and researcher, used fMRI to show in six volunteers that stimulation of two different points on the auricle activated two different brain areas consistent with the proposed regions on the auricular maps (18).
Besides the cartography of auriculotherapy proposed by Nogier in 1957 and the standardization of auricular acupuncture points proposed by the Chinese in the late 1970s, the World Health Organization (WHO), after an 8-year effort of revisions with the collaboration of reference professionals in the area around the world, also recognized and systematized the auricular acupuncture microsystem (19,20). Furthermore, Dr. Oleson also has published many works on auricular acupuncture, including the Auriculotherapy Manual: Chinese and Western Systems of Ear Acupuncture and the International Handbook of Ear Reflex Points, and he presented his work on standardized auricular nomenclature at meetings of the WHO in 1990, a hybrid map with points from Chinese and French cartography (11).
The process of standardizing the auricular points was later carried out by Chinese researchers and the final document was published in 1993 and confirmed in 2008 (21). The final document is a hybrid with Nogier’s considerations of nervous system points, contributions from the Chinese academic consensus, the map proposed by the WHO, and the nomenclature system previously proposed by Oleson. In fact, the use of ear points in Europe still differs from the Chinese practice, but it should be noted that the current Chinese maps correspond faithfully to Nogier’s historical maps (22).
Thus, the international pattern of distribution and location of the auricular acupuncture points; Chinese pattern, adopted by the World Federation of Acupuncture and Moxibustion Societies (WFAS); is based on sub-areas using the anatomy of the pinna in the form of an acronym followed by a number forming quadrants (Figure 2) (19-23). The standardization of the WFAS map was revised again in 2012 with the approval of an international working group, including experts from China, America, Canada, Iran, and South Korea, and then published in 2013 (24,25).
The auricular cartography proposed by Nogier has served as a theoretical reference for several auricular maps, including the Chinese auricular acupuncture map. Auricular maps are the basis for the practical location of points. In addition, Nogier, Bourdiol, and Bahr in 1981 created the concept of auriculomedicine, based mainly on a vascular reflex perceived during palpation of the radial artery while performing an auricular examination, called vascular autonomic signal, which helps in locating the auricular points by identifying the immediate responses of the autonomic nervous system upon stimulation of auricular points (15). Other methods to aid the identification of ear points and their interface with the nervous system have also been studied. In 1963, Niboyet proposed measuring the electrical impedance of the skin surface taking into consideration the location of the Chinese points (15). Clinically, this resource has been tested for the identification of auricular points with low electrical impedance in cases of orthopedic and organic dysfunctions (26-29).
The continuous development of auriculotherapy currently requires an update of its international standardization. Alimi and Chelly proposed a biomathematical model of the neuroanatomical organization of the brain based on neuroembryological and neurophysiological data, upon which the auricular pavilions are connected. The World Federation of Chinese Medicine Societies (WFCMS) ratified the model during its 8th Convention in London with the participation of Dr. Qi Zhang, Coordinator of the Department of Traditional Medicine, at WHO. This International Nomenclature of Auriculotherapy allows homogeneity in the fields of education, research and publication, and may facilitate the work of auriculotherapists and allow scientific progress of the subject worldwide (30).
The 8th ISO/TC249 Plenary Meeting, which occurred in 2019, brought together more than two hundred delegates, who came from over 13 countries including China, Australia, the United States, Canada, Japan, South Korea, Thailand and A-level liaison organizations included in WFAS. At that meeting, there was a discussion about the project “General requirement for the risk control in the safe use of acupuncture”. In addition, delegates from WFAS committed to continuing playing its role of A-level liaison organization and actively participating in setting of topics, techniques and international tool standards of acupuncture-moxibustion in ISO/Technical Committee.
In Brazil, the European Foundation of Traditional Chinese Medicine collaborated with the regulation of acupuncture, noting the WHO strongly recommends the regulation of traditional and complementary medicine (T&CM) and their integration into the National Health Systems in the WHO Traditional Medicine Strategy: 2014–2023 (WFAS).
Translational medicine
For a long time now, basic research carried out with laboratory animals and clinical practice have developed in parallel in their respective forms in various fields. However, translational medicine aims to bridge the gap between them, to apply the latest findings of basic research to clinical practice quickly and efficiently. Furthermore, translational medicine can translate research results into techniques, methods and medicines for disease prevention, diagnosis and assessment of patient prognosis (30,31). The auricle in humans and other mammals has a special anatomical structure, that is, there is a branch of the vagus nerve distributed in the shell (32,33). In fact, most of the information about the anatomy of the vagus nerve and its projections was discovered by tracing the vagus nerve in rats and is generally considered to be similar to humans (33).
An animal model for auricular acupuncture was described by Ng et al. in rats in 1975. In animals, because no criteria had been established to provide guidelines as to the effectiveness of the acupuncture procedure, such as the presence of “De Qi” in humans, the researchers observed a behavioral signal. In these rodents, it was found that applying strong pressure, particularly to the concha or crus area of the ear, could induce a state of behavioral inhibition similar to the state of behavioral inhibition observed in a variety of animal species under certain sensory manipulations. Furthermore, the authors found that this state of behavioral inhibition could be maintained for considerable periods if a rhythmic, low-intensity, low-frequency stimulus was applied and if handling and disturbing noise were kept to a minimum. Using this information, the research group developed what they considered to be the first animal model for auricular electroacupuncture (34,35).
Gao et al. (36) in 2008 systematically analyzed the location specificity and response characteristics of autonomic changes using different stimulation methods in auricular acupuncture in rats. The authors showed that stimulation of the auricle with either manual or electroacupuncture (100 Hz–1 mA) was able to decrease blood pressure, causing bradycardia and gastric contraction. The study suggested that the inferior concha is the most powerful site for regulation of autonomic functions, at least in animals.
Currently, there are many authors researching acupuncture treatment and, especially auricular electroacupuncture. Some preliminary preclinical evidence suggests that auricular stimulation of the vagus nerve may reduce the inflammatory response through activation of the cholinergic anti-inflammatory pathway, playing a key role in peripheral cholinergic release and inflammation suppression (37-39). Constant bilateral stimulation of the vagus nerve led to less food intake and sweet cravings in obese mini pigs, suggesting that the treatment helps prevent excess weight gain. The exact mechanism by which auricular stimulation of the vagus nerve influences weight loss is still unknown, but it is believed that changes in metabolism, decreases in fat stores or changes in satiety signaling may occur (40,41). In an ischemia/reperfusion rat model, the authors showed that auricular stimulation of the vagus nerve improved cardiac function and reduced infarct size. In addition, the treatment reduced mesenteric artery damage and vasodilation caused by the ischemia/reperfusion model, also decreasing blood cytokine levels (42). Spontaneously hypertensive rats with high salt content diet treated with auricular stimulation of the right vagus nerve did not present aortic stiffening and had a delay in the progression of endothelial dysfunction (43).
In addition to studies targeting peripheral conditions, a relevant number of publications with models of depression have been published. This is a clinical condition that can be seen in isolation or sharing a high degree of comorbidity with other diseases. In rats, the transcutaneous auricular vagus nerve stimulation (taVNS) has been shown to be able to reverse depressive-like behavior and reduce the concentration of TNF-α in plasma, prefrontal cortex (PFC), hippocampus, amygdala and hypothalamus (44). Still in rats models of depression, the taVNS at 2/15 Hz at 2 mA, for 30 minutes/day and for 21 days, was also able to reverse depression-like behavior and hippocampal neuroinflammation, with downregulation of α7nAchR and upregulation of NF-κB p65 and IL-1β (45). In this sense, taVNS had antidiabetic and antidepressant effects in diabetic and fatty Zucker rats, reducing the expression of limbic-regional P2X7R. These animals, compared to lean rats, have elevated limbic-regional P2X7R (46).
The basic research mentioned above supports the theory of the pathway connecting the points of the ear with the vagus nerve from different angles. However, there are many difficulties in translating basic research findings, especially due to insufficient incentives and inadequate evaluation of results, high costs, lack of deep and efficient communication between researchers from research institutions and clinicians or pharmaceutical companies. The disconnect between clinical work and basic research makes it even more difficult to commercialize and apply the achievements of many scientific research projects (30,31).
Neuromodulation and auricular acupuncture
Possibly, one of the great impulses for the increasing interest of the scientific community in auricular therapeutic approaches was the investment of science in researching the role of the vagus nerve in the constant search for balance in the internal environment, that is, its role in homeostasis. There is a growing number of publications on vagal stimulation in the treatment of conditions such as chronic pain, depression and epilepsy. The fact that the central concha of the auricula is the only external region of the body with free access to the vagus nerve, makes the auricular pavilion a good option for this type of therapy, considering the possible adverse events of invasive vagal stimulation, such as hoarseness, cough and dyspnea, in addition to the other risks of a surgical procedure (47,48).
The first record showing a possible auricular branch of the vagus nerve (ABVN) was made by the German anatomist Friedrich Arnold in 1832, when he observed that it was possible to stimulate the cough reflex through the auditory canal. Later, around 1984, researchers Nomura and Mizuno published a study carried out on cats that showed the relationship of innervation of the auricular concha’s skin with the nucleus of the solitary tract (NTS), thus establishing the ABVN. Long before that, studies with vagal stimulation and its changes in brain function were also done in cats, by researchers Bailey in 1938 and soon after with primates, by Dell and Olson in 1951, showing their effects on limbic regions of the thalamus and cingulate cortex, thus raising the hypothesis that this type of stimulation may have anticonvulsant effects (2,47,48).
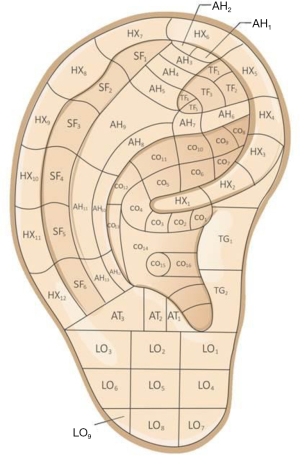
In 2002, Punker and Filler published a study performed on cadavers where they mapped the auricular innervation, showing the distribution of cranial nerves predominantly in the central concha and spinal nerves in the periphery of the pavilion (Figure 3). It is an intertwined nervous network that is confused throughout the extension of the auricle, but with a predominance of some nerves that reach 100% in some regions, such as the ABVN over the cymba conchae and the great auricular nerve over the region of the helix tail and scapha (49).
The cranial nerves, including ABVN and the auriculotemporal nerve, which is a branch of the trigeminal nerve, cover the central part of the auricula, connect to the central nervous system through the bulb, the lower region of the brainstem that controls autonomic functions related to breathing, heart rate, blood pressure, gastrointestinal activities and some reflexes such as swallowing, coughing, sneezing and vomiting; in addition, this region has nuclei that connect with limbic structures and descending control nuclei of nociceptive information—forming the descending inhibitory pathway (50,51).
Spinal nerves arise from the second and third pairs of spinal nerves of the cervical plexus and form the great auricular nerve and the minor occipital nerve. They reach the auricle through its posterior face, where they have larger ramifications. On the anterior face of the pavilion, they cover the external or peripheral region of the auricle. Possibly, they are related to activation of the descending inhibitory pathways of nociception. In fact, most studies with auricular neuromodulation target the trigeminal and vagal branches, while the auricular areas innervated predominantly by the cervical plexus are used as controls in research (48).
Until recently, ABVN’s projections for brain circuits from the NTS in humans were nothing more than plausibility derived from preclinical studies carried out in felines and rodents. The first evidence in humans was published in 2015, when Eleni Frangos and collaborators showed circuits activated from the stimulation of ABVN covering the midbrain, limbic structures and the somatosensory cortex through fMRI (51). Thus, possibly the antinociceptive effects shown in studies with ABVN stimulation are consistent with the activation of the periaqueductal gray matter, dorsal raphe nucleus and locus coeruleus, which are part of the descending inhibitory pathways. Antidepressant effects, also evidenced by some studies, may be related to activation of the amygdala and nucleus accumbens. Similarly, anticonvulsant effects of ABVN stimulation seem to be related to the deactivation of the hippocampus (51).
Finally, a review of the neurophysiological effects of electrical stimulation of ABVN analyzed by fMRI, published in 2018 by Badran et al. (52), showed that the results vary widely in terms of activation and inhibition of brain regions, variation possibly related to the diversity of methods presented in different studies, including the auricular region, intensity, stimulus frequency and current pulse width, since studies use electrical stimulation.
Discussion
Auricular therapy has two major methodological lines, one is the European pattern developed by Nogier and baptized as auriculotherapy, the other is the oriental pattern proposed by the Chinese, recognized as auricular acupuncture. These two lines have some differences regarding the nomenclature of points and the localization of some auricular points, the biggest one is the localization of the lower limb: while in the occidental line the lower limb is located on the triangular fossa, the oriental map localizes it on the superior cross of the antihelix (25). In addition, several cartographies were created by different authors along the spread of both lines of auricular therapy around the world, independently and based on clinical experience, outside a controlled research environment and without peer-review (15). This diversity of maps contributes to challenges for teaching and lack of consensus and credibility of auricular therapy (15,25). Our review emphasized the Chinese pattern and its standardization published by WFAS in an effort to urge auricular therapy specialists to use an international standardization, thereby facilitating clinical and academic communication.
Basic science studies contribute to the understanding of the potential neurobiological mechanisms involved in auricular therapy, supporting a biological plausibility of this therapeutic method. These studies also serve as an incentive to develop further human studies, validating the preclinical evidence (15). This review has shown an overview of the empirical development of auricular therapy and the quest of science to explore its biological plausibility.
Finally, we explore the evidence supporting the use of auricular therapy as a neuromodulation tool, employed primarily in chronic conditions such as pain and depression. However, neuromodulation by auricular therapy may be another way to think and support what was already proposed by auricular acupuncture (53).
Our study is a narrative review that can provide the reader an overview of the state of the art of auricular acupuncture and neuromodulation. However, we know that narrative reviews are not critical and have a number of limitations. In this sense, our review worked with a single database, and even though the authors were free to access secondary databases if they needed to, this is a limitation. We also only accessed English language publications, leaving out, for example, Chinese studies. Thus, it is possible that important studies were not selected, which is another limitation. Even so, we believe that our review can contribute as a synthesis of the history and main evidence for auricular acupuncture and neuromodulation.
Conclusions
Experimental and clinical studies analyzing data from animals and humans can establish the role of cranial and cervical spinal nerves in some of the mechanisms of pain neuromodulation, especially in relation to the ABVN. Stimulation in adequate doses on the central and peripheral regions of the auricular pavilion can trigger behavioral inhibition effects, reduce inflammatory response and appetite, improve cardiac function, depressive symptoms, epilepsy and pain.
Discussing the mechanism of functioning and clinical efficacy of auricular acupuncture based on basic experimental research and preliminary pre-clinical experiments can provide strong scientific support for the clinical application of the technique and improvement of the therapeutic method. Therefore, continuous joint effort of researchers and clinicians is needed, searching for a cost-effective treatment, based on quality studies and research protocols.
Acknowledgments
Funding: This article was supported by Neuroscience Post-Graduate Program at the Federal University of Santa Catarina (UFSC) and financial support from National Council for Scientific and Technological Development (CNPq), Foundation for the Support of Research and Innovation of the State of Santa Catarina (FAPESC), Coordination for the Improvement of Higher Education Personnel (CAPES), and INCT-INOVAMED Program (465430/2014-7) grants.
Footnote
Provenance and Peer Review: This article was commissioned by the editorial office, Longhua Chinese Medicine for the series “Ear Acupuncture Neuromodulation”. The article has undergone external peer review.
Reporting Checklist: The authors have completed the Narrative Review reporting checklist. Available at https://lcm.amegroups.com/article/view/10.21037/lcm-21-42/rc
Peer Review File: Available at https://lcm.amegroups.com/article/view/10.21037/lcm-21-42/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://lcm.amegroups.com/article/view/10.21037/lcm-21-42/coif). The series “Ear Acupuncture Neuromodulation” was commissioned by the editorial office without any funding or sponsorship. MLN served as the unpaid Guest Editor of the series. The authors have no other conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Gori L, Firenzuoli F. Ear acupuncture in European traditional medicine. Evid Based Complement Alternat Med 2007;4:13-6. [Crossref] [PubMed]
- Hou PW, Hsu HC, Lin YW, et al. The History, Mechanism, and Clinical Application of Auricular Therapy in Traditional Chinese Medicine. Evid Based Complement Alternat Med 2015;2015:495684. [Crossref] [PubMed]
- Wirz-Ridolfi A. The History of Ear Acupuncture and Ear Cartography: Why Precise Mapping of Auricular Points Is Important. Med Acupunct 2019;31:145-56. [Crossref] [PubMed]
- Brazil. Ministry of Health. Department of Health Care. Department of Primary Care. National Policy on Integrative and Complementary Practices in the SUS – PNPIC-SUS. Brasília: Ministry of Health, 2006. Available online: http://bvsms.saude.gov.br/bvs/publicacoes/politica_nacional_praticas_integrativas_complementares_2ed.pdf
- Colvin L, Atherton R, Bannister J, et al. Scottish Intercollegiate Guidelines Network (SIGN). Management of chronic pain. Edinburgh: SIGN, 2019.
- He Y, Guo X, May BH, et al. Clinical Evidence for Association of Acupuncture and Acupressure With Improved Cancer Pain: A Systematic Review and Meta-Analysis. JAMA Oncol 2020;6:271-8. [Crossref] [PubMed]
- Murakami M, Fox L, Dijkers MP. Ear Acupuncture for Immediate Pain Relief-A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pain Med 2017;18:551-64. [PubMed]
- Asher GN, Jonas DE, Coeytaux RR, et al. Auriculotherapy for pain management: a systematic review and meta-analysis of randomized controlled trials. J Altern Complement Med 2010;16:1097-108. [Crossref] [PubMed]
- Veith I. The Yellow Emperor’s Classic of Internal Medicine. Berkeley, CA, USA: University of California Press, 1972.
- Huang H. Ear Acupuncture. Emmaus, PA, USA: Rodale Press, 1974.
- Oleson T. Auriculotherapy Manual. 4th edition. Toronto: Elsevier, 2013.
- Zang Z. Essential Techniques for Massage, Beijing: People’s Medical Publishing House, 1955.
- Nogier P. From Auriculotherapy to Auricular Medicine. Sainte-Ruffine: Maisonneuve, 1981.
- Landgren K. Ear Acupuncture: A Practical Guide. London: Churchill Livingstone, 2008.
- Rabischong P, Terral C. Scientific Basis of Auriculotherapy: State of the Art. Med Acupunct 2014;26:84-96. [Crossref] [PubMed]
- Oleson TD, Kroening RJ, Bresler DE. An experimental evaluation of auricular diagnosis: the somatotopic mapping of musculoskeletal pain at ear acupuncture points. Pain 1980;8:217-29. [Crossref] [PubMed]
- Alimi D, Geissmann A, Gardeur D. Auricular Acupuncture Stimulation Measured On Functional Magnetic Resonance Imaging. Med Acupunct 2002;13:18-21.
- Romoli M, Allais G, Airola G, et al. Ear acupuncture and Fmri: a pilot study for assessing the specificity of auricular points. Neurol Sci 2014;35:189-93. [Crossref] [PubMed]
- Zhao B, Meng X, Sun J. An Analysis of the Development of Auricular Acupuncture in China in the Past 10 Years. Med Acupunct 2018;30:133-7. [Crossref] [PubMed]
- WHO. Report of the Working Group on Auricular Acupuncture Nomenclature. France: World Health Organization, 1991.
- Technical Supervise Bureau of State, The Nomenclature and Location of Ear Acupuncture Points. Beijing: Chinese Standard Publishing House, 2008.
- Romoli M. Ear acupuncture: historical abstract-differences of ear cartography between the east and the west. Dtsch Zeitschrift für Akupunkt 2010;53:24-33. [Crossref]
- Rong PJ, Zhao JJ, Wang L, et al. Analysis of Advantages and Disadvantages of the Location Methods of International Auricular Acupuncture Points. Evid Based Complement Alternat Med 2016;2016:2806424. [Crossref] [PubMed]
- World Federation of Acupuncture-Moxibustion Societies (WFAS). Auricular acupuncture point (WFAS STANDARD-002: 2012). World J Acupunct-Moxibustion 2013;23:12-21. [Crossref]
- Wang L, Yanga J, Zhao B, et al. The similarities between the World Federation of Acupuncture Moxibustion Societies’ standards for auricular acupuncture points and the European System of Auriculotherapy Points according to Nogier and Bahr. Eur J Integr Med 2016;8:817-34. [Crossref]
- Usichenko TI, Lysenyuk VP, Groth MH, et al. Detection of ear acupuncture points by measuring the electrical skin resistance in patients before, during and after orthopedic surgery performed under general anesthesia. Acupunct Electrother Res 2003;28:167-73. [Crossref] [PubMed]
- Romoli M, Mazzoni R. The Validation of Auricular Diagnosis. Deutsche Zeitschrift für Akupunktur 2009;52:10-6. [Crossref]
- Cheing GL, Wan S, Lo SK. The use of auricular examination for screening hepatic disorders. J Acupunct Meridian Stud 2009;2:34-9. [Crossref] [PubMed]
- Suen LK, Yeh CH, Lee WK, et al. Association of auricular reflective points and the status of lower urinary tract symptoms in aging males. Aging Male 2015;18:149-56. [Crossref] [PubMed]
- Alimi D, Chelly JE. New Universal Nomenclature in Auriculotherapy. J Altern Complement Med 2018;24:7-14. [Crossref] [PubMed]
- Rong PJ, Zhao JJ, Li YQ, et al. Auricular acupuncture and biomedical research--A promising Sino-Austrian research cooperation. Chin J Integr Med 2015;21:887-94. [Crossref] [PubMed]
- Zhao YX, He W, Jing XH, et al. Transcutaneous auricular vagus nerve stimulation protects endotoxemic rat from lipopolysaccharide-induced inflammation. Evid Based Complement Alternat Med 2012;2012:627023. [Crossref] [PubMed]
- Chung WY, Zhang HQ, Zhang SP. Peripheral muscarinic receptors mediate the anti-inflammatory effects of auricular acupuncture. Chin Med 2011;6:3. [Crossref] [PubMed]
- Ng LK, Douthitt TC, Thoa NB, et al. Modification of morphine-withdrawal syndrome in rats following transauricular electrostimulation: an experimental paradigm for auricular electroacupuncture. Biol Psychiatry 1975;10:575-80. [PubMed]
- Ng LK. Auricular acupuncture in animals: effects of opiate withdrawal and involvement of endorphins. J Altern Complement Med 1996;2:61-3; discussion 73-5. [Crossref] [PubMed]
- Gao XY, Zhang SP, Zhu B, et al. Investigation of specificity of auricular acupuncture points in regulation of autonomic function in anesthetized rats. Auton Neurosci 2008;138:50-6. [Crossref] [PubMed]
- Tracey KJ. The inflammatory reflex. Nature 2002;420:853-9. [Crossref] [PubMed]
- Borovikova LV, Ivanova S, Zhang M, et al. Vagus nerve stimulation attenuates the systemic inflammatory response to endotoxin. Nature 2000;405:458-62. [Crossref] [PubMed]
- Matteoli G, Gomez-Pinilla PJ, Nemethova A, et al. A distinct vagal anti-inflammatory pathway modulates intestinal muscularis resident macrophages independent of the spleen. Gut 2014;63:938-48. [Crossref] [PubMed]
- Bodenlos JS, Kose S, Borckardt JJ, et al. Vagus nerve stimulation acutely alters food craving in adults with depression. Appetite 2007;48:145-53. [Crossref] [PubMed]
- Val-Laillet D, Biraben A, Randuineau G, et al. Chronic vagus nerve stimulation decreased weight gain, food consumption and sweet craving in adult obese minipigs. Appetite 2010;55:245-52. [Crossref] [PubMed]
- Zhao M, He X, Bi XY, et al. Vagal stimulation triggers peripheral vascular protection through the cholinergic anti-inflammatory pathway in a rat model of myocardial ischemia/reperfusion. Basic Res Cardiol 2013;108:345. [Crossref] [PubMed]
- Chapleau MW, Rotella DL, Reho JJ, et al. Chronic vagal nerve stimulation prevents high-salt diet-induced endothelial dysfunction and aortic stiffening in stroke-prone spontaneously hypertensive rats. Am J Physiol Heart Circ Physiol 2016;311:H276-85. [Crossref] [PubMed]
- Guo X, Zhao Y, Huang F, et al. Effects of Transcutaneous Auricular Vagus Nerve Stimulation on Peripheral and Central Tumor Necrosis Factor Alpha in Rats with Depression-Chronic Somatic Pain Comorbidity. Neural Plast 2020;2020:8885729. [Crossref] [PubMed]
- Wang JY, Zhang Y, Chen Y, et al. Mechanisms underlying antidepressant effect of transcutaneous auricular vagus nerve stimulation on CUMS model rats based on hippocampal α7nAchR/NF-Kb signal pathway. J Neuroinflammation 2021;18:291. [Crossref] [PubMed]
- Yu Y, He X, Wang Y, et al. Transcutaneous auricular vagal nerve stimulation inhibits limbic-regional P2X7R expression and reverses depressive-like behaviors in Zucker diabetic fatty rats. Neurosci Lett 2022;775:136562. [Crossref] [PubMed]
- Mercante B, Deriu F, Rangon CM. Auricular Neuromodulation: The Emerging Concept beyond the Stimulation of Vagus and Trigeminal Nerves. Medicines (Basel) 2018;5:10. [Crossref] [PubMed]
- Mercante B, Ginatempo F, Manca A, et al. Anatomo-Physiologic Basis for Auricular Stimulation. Med Acupunct 2018;30:141-50. [Crossref] [PubMed]
- Peuker ET, Filler TJ. The nerve supply of the human auricle. Clin Anat 2002;15:35-7. [Crossref] [PubMed]
- Napadow V, Edwards RR, Cahalan CM, et al. Evoked pain analgesia in chronic pelvic pain patients using respiratory-gated auricular vagal afferent nerve stimulation. Pain Med 2012;13:777-89. [Crossref] [PubMed]
- Frangos E, Ellrich J, Komisaruk BR. Non-invasive Access to the Vagus Nerve Central Projections via Electrical Stimulation of the External Ear: Fmri Evidence in Humans. Brain Stimul 2015;8:624-36. [Crossref] [PubMed]
- Badran BW, Dowdle LT, Mithoefer OJ, et al. Neurophysiologic effects of transcutaneous auricular vagus nerve stimulation (taVNS) via electrical stimulation of the tragus: A concurrent taVNS/Fmri study and review. Brain Stimul 2018;11:492-500. [Crossref] [PubMed]
- Kong J, Fang J, Park J, et al. Treating Depression with Transcutaneous Auricular Vagus Nerve Stimulation: State of the Art and Future Perspectives. Front Psychiatry 2018;9:20. [Crossref] [PubMed]
Cite this article as: Neves ML, Coutinho BD, da Silva EDC, Gentil LB, dos Santos ARS, da Silva MD. Ear acupuncture and neuromodulation: narrative review. Longhua Chin Med 2022;5:27.