Effectiveness of electroacupuncture for a patient with a complete traumatic spinal cord injury: a case report
Introduction
Spinal cord injury (SCI) is one of the most prevalent causes of disease and disability worldwide, and the sequels include serial complications in patients like disability and serial complications (1).
Traumatic SCI is accompanied by substantial acute and recurrent morbidity and raised mortality (1,2). The chronic course of the condition is dominated by the loss of motor and sensory function, but also includes symptoms such as autonomic dysreflexia and impairment of bowel and bladder control as well as pain and spasticity resulting in significant loss of quality of life. In the acute phase of traumatic SCI, surgical treatment targeting spine stability and decompression is often opted for, although a conservative approach may be chosen as well (3,4).
Studies have suggested that the surgical impact on neurological improvement is marginal in complete traumatic SCI (4-6).
Investigation shows that subjects with SCI sequels are recurrently interested in acupuncture and holistic medicine for symptomatic relief (7-9).
Based on traditional Chinese medicine used for more than four thousand years, acupuncture is an essential part that has been used to treat a variety of diseases all over the years. It consists of the insertion of needles into specific body points (acupoints) for activating the energy flow, also known as Qi, to balance the flow of the energy which contributes to treating, maintaining and preventing diseases (10).
Scientific research has shown that acupuncture can stimulate nerve regeneration and improve nerve conduction in injured nerves (11).
Chinese Medicine, via the application of acupuncture, manual therapy and moxibustion, had been recommended due to their effect, cost-effectiveness, safety and simplicity of operation for treating the sequels of injured nerves. Numerous studies focus on the treatment of neurogenic bladder dysfunction after a SCI, showing that electroacupuncture (EA) treatment has no related risks or medication side effects, often seen with long term usage of pharmaceutical medications (12).
Even if conservative treatments are suggested at the beginning, some patients do not respond to conservative treatments and need more surgical interventions over time, there are ongoing clinical trials to assess clinical Effects, Brain Structural and Functional Changes on Spinal Cord Injury (NCT03909958) (13-15).
Clinical experience suggests that acupuncture can be efficient when the needle is introduced anywhere at motor point or in the appropriate segment (13,14). Needles may be hand stimulated, by electric current or by warmth. The depth or gauge of the needle are not so relevant, studies show that the duration of the treatment contributes much more to the acupuncture efficacy (1,12).
Nevertheless, there is a lack of research in the current literature supporting the use of EA as an adequate intervention for SCI. The objective of this case report was to describe the acute effects of EA as a treatment intervention for an individual with a complete SCI. We present the following case in accordance with the CARE reporting checklist (available at https://lcm.amegroups.com/article/view/10.21037/lcm-21-69/rc)
Case presentation
The individual in this study is a 32-year-old woman without any pre-existing medical condition and a history of a complete SCI subsequent to an accident landing on her back when falling off a roof from a height of 3 meters in May 2018. The initial computerized tomography (CT) examination after the injury indicates: complete L1 crack fracture, upper plat L2 fracture, posterior elements of T12 fractured, displaced sacrococcygeal fracture.
The diagnosis was a complete T10 SCI Asia A (American Spinal Injury Association) and no motor and sensory function from L1 to S3 secondary to a L1 fracture.
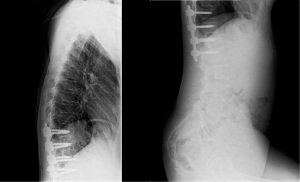
The patient underwent an emergency surgery to stabilize the fracture. It was stabilized with posterior instrumentation from T10 to L1 (Figure 1). The patient stayed at the hospital for her recovery and was discharged in October 2018. The patient started physical therapy rehabilitation on 1st October 2018, conservative treatment was applied in order to improve range of motion, enhance muscle activation, re-educate transfers and daily activities and training with a wheelchair.
Evolution was positive and in February 2019 (Table 1) the patient was discharged with the following outcomes:
Table 1
| Date | Event |
|---|---|
| May 2018 | Injury |
| October 2018 | Hospital discharge |
| Starts physical rehabilitation | |
| February 2019 | Physical rehabilitation discharge (Institut Guttmann) |
| May 2019 | Initiates EA treatment |
| April 2020 | Medical report with positive outcomes |
EA, electroacupuncture.
The patient started physical rehabilitation in May 2019. After one year of physical rehabilitation with no significant outcomes, the patient decided to start acupuncture sessions.
In February 2020 she initiates her acupuncture treatment, at this moment the outcomes are similar than in February 2019 (Table 2), with urinary incontinence and the same motor outcomes.
Table 2
| JM | PROM (R/L) | MB (R/L) |
|---|---|---|
| Hip flexion | 120º/115º | 4/4 |
| Hip extension | 15º/15º | 1/1 |
| Hip abduction | 42º/33º | 3/4 |
| Hip external rotation | 24º/33º | 3/3 |
| Knee flexion | 120º/120º | 2/2 |
| Knee extension | 0º | 4/3 |
| Knee internal rotation | 30º/30º | 2/2 |
| Knee external rotation | 54º/49º | 3/3 |
| Ankle plantar flexion | 10º/12º | 1/1 |
| Ankle plantar extension | 5º/7º | 1/1 |
JM, joint mobility; PROM, passive range of motion; MB, muscular balance; R/L, right/left.
She was not doing physical therapy at that moment because she had no financial resources and it was not included in her social insurance. She practiced physical activity on her own: swimming and gym, twice a week.
At that moment, the patient was treated with neuroleptics for depression. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Therapeutic intervention
The patient underwent one hour EA session per week during 12 months.
Needles were inserted bilateral, with the purpose of invoking a nearly strong yet bearable qi sensation. Subsequently, needles were connected for electrical stimulation using low-frequency (5 Hz) continuous waves for 28 min. The output intensity was adjusted to the maximum allowed by the patient, and was assisted by EA-induced rhythmic local muscle contractions.
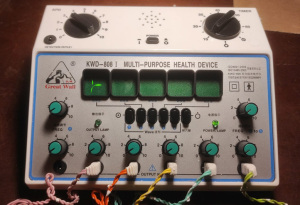
The electric stimulation device applied was a portable “Great Wall” low-frequency stimulator (Model KWD-808), 6 channel Transcutaneous Electrical Nerve Stimulation (TENS) unit (Figure 2).
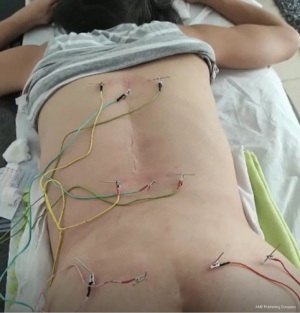
Low intensity and continuous current of 5 Hz applied following the energy flow of the Bladder Vessel, positive poles towards the caudal. The electrodes were connected in parallel (Figure 3).
Two additional acupuncture points manually stimulated (62B, 3SI) were treated to increase the effects of acupuncture on the Governing Vessel (GV) (Table 3).
Table 3
| Acupoint | Location | Needle depth | Stimulation |
|---|---|---|---|
| 9GV TSE YANG | Inferior depression of D7 spinous process | 0.7 Cun | 5 Hz, − pole |
| 18B KAN LU | On the sides of D7 spinous process | 1.5 Cun | 5 Hz, − pole |
| 3GV YANG KOANN | Inferior depression of L4 spinous process | 0.7 Cun | 5 Hz, + pole |
| 25B TA TCHANG LU | On the sides of L4 spinous process | 1.5 Cun | 5 Hz, + pole |
| 30B BAI HUAN SHU | 1.5 Cun from spine on the sides of S4 | 1 Cun | 5 Hz, − pole |
| 54B TCHÉ PIEN | 3 Cun from spine on the sides of S4 | 1.5 Cun | 5 Hz, + pole |
| 31GB FONG CHÉ | Thigh outer face 7 Cun above knee joint | 1.5 Cun | 5 Hz, − pole |
| 34GB YANG LIN TSIUAN | Anterior and distal depression of the fibula head | 1 Cun | 5 Hz, + pole |
| 55B JO YANG | 2 Cun below popliteal fossa | 1.5 Cun | 5 Hz, − pole |
| 60B KUEN LOUN | Between outer ankle knuckle and Achilles heel | 0.5 Cun | 5 Hz, + pole |
| 62B CHEN MO | Outer ankle knuckle distal depression | 0.3 Cun | Manual stimulation |
| 3SI JEOU TSI | Ulnar aspect of the hand | 0.5 Cun | Manual stimulation |
Acupoint: GV, governing vessel; B, bladder; GB, gallbladder; SI, small intestine. +, positive pole; −, negative pole.
After seven months, superficial moxibustion of limbs was included and combined with electrostimulation.
Follow-up and outcomes
The individual well-tolerated EA sessions and underwent one hour session per week regularly during one year.
The primary outcome is the difference in urinary symptoms before and after treatment, stated by the patient and by a medical report in April 2020. The patient gained complete bladder control.
In April 2021 the diagnosis was stated as Incomplete SCI (T12 sensory and L3 motor).
The secondary outcomes include the following items:
- Improvements in muscular balance (MB): the patient reported better control and strength in proximal lower limb muscles: psoas, quadriceps, hamstrings, abductor, tibialis and gastrocnemius. Outcomes were measured using Oxford scale (Table 4).
Table 4
Outcome measures. Oxford’s scaleJM PROM (R/L) MB (R/L) Hip flexion 125º/122º 4/4 Hip extension 17º/18º 2+/2 Hip abduction 45º/39º 3/4 Hip external rotation 28º/36º 3/3 Knee flexion 120º/120º 2/2 Knee extension 0º 5/4+ Knee internal rotation 30º/30º 3/3 Knee external rotation 64º/58º 3/3 Ankle plantar flexion 18º/16º 0/0 Ankle plantar extension 10º/10º 0/0 +, slight improvement. JM, joint mobility; PROM, passive range of motion; MB, muscular balance; R/L, right/left. - Improvements in passive range of motion: the patient reported better hip, knee and ankle joint mobility. Outcomes were measured with a common goniometer (Tables 4,5
). Table 5
Improvement percent pre and post interventionJM % Improvement R % Improvement L Hip flexion 4.17 6.09 Hip extension 13.33 20 Hip abduction 7.14 18.18 Hip external rotation 16.67 9.09 Knee flexion 0 0 Knee extension 0 0 Knee internal rotation 0 0 Knee external rotation 18.52 18.37 Ankle plantar flexion 80 33.33 Ankle plantar extension 100 42.86 JM, joint mobility; R, right; L, left. - Improvements in walk ability: the patient is able to stand and walk 3 meters for a few seconds without help.
Discussion
The purpose of this case was to demonstrate the efficacy of EA treatment for an individual with a complete SCI. The subject demonstrates positive clinical outcomes after 12 months of treatment of which the most relevant is the recovery of a complete bladder control, improvements in joint mobility and MB were also observed.
This case report uses only a single individual, as is typical of a case report research (16-18). This is an intrinsic limitation to a case report, showing only results related to one individual that cannot be summarized. More randomized control studies about SCI interventions are needed in order to fully determine the effectiveness of EA as a primary intervention for SCI.
Clinical research indicated that acupuncture therapy can improve maximum bladder compliance and bladder capacity (18). In addition, EA can relieve overactive bladder symptoms, including the first urge to void, first sensation of bladder filling and maximum cystometric scope (18,19).
Notably, the management of neurogenic bladder after SCI based on the basic principles of acupuncture and moxibustion therapies, shows that stimulating acupuncture points to regulate the physiological function of the bladder may be effective (20).
Many studies have been conducted previously to evaluate the potency of available symptom-relief interventions. While most of preceding systematic reviews and meta-analyses were focusing on the efficacy and safety of acupuncture in relieving urinary symptoms, there are lack of rankings of efficacy or comparisons among the presently accessible acupuncture and moxibustion therapies for neurogenic bladder due to SCI (12,13,19).
EA is an unrecognized, safe and potential nonpharmacological intervention that has a short-term positive effect on the release of many substances including endorphins.
Although the effect duration is short (approximately 1 day), EA may accelerate tissue metabolism and recovery to induce a long-term treatment effect for injured nerves (10,11).
Previous reviews provided evidence for the safety and efficacy of acupuncture therapy for complications after SCI and concluded that the positive effects appear to result from improvement of neuroplasticity, reduction of inhibition of inflammation, regulation of the expression and activity of endogenous biological mediators, promotion of regenerative stem cells, oxidative stress and neuronal apoptosis (7).
Other studies stated that the acupuncture effects are a result from stimulation of appropriate spinal cord segmental levels or peripheral nerves, and the release of endogenous opioids at the spinal cord level produced by acupuncture treatment and electrical stimulation of peripheral nerves ensure its effects in pain relief and limiting SCI after acute trauma (2).
However, to ensure unbiased study results it is important to note that double-blind trials are needed due to the methodological weaknesses of the previous clinical trials. Older studies, prior to 2000 tend to be more anecdotal and do not provide the detailed methodologic data, but can provide guidance for treatment (7,20).
Conclusions
This case report described the treatment of an individual with a complete SCI using EA. The subject of this research tolerated the EA treatment, demonstrating clinically meaningful improvements in bladder control and motor skills, without short-term adverse effects. The outcomes from this case report indicate that EA may be effective in the treatment of SCI when the presentation includes the bladder control loss and lower limbs weakness.
Studies with supplementary assessment periods designed to investigate longer term versus short-term benefits of EA need to be conducted. Complementary research is recommended to determine if EA is clinically beneficial separate of other therapeutic interventions such as specific or general exercises focusing the affected musculature, or other manual therapy techniques such as soft tissue mobilization massage.
Considering the lack of any controls in this case, we cannot establish any definitive conclusions regarding the effectiveness of EA in SCI. Larger randomized controlled trials are required to verify EA utility for this indication, including an adequate sample size and a control group to explore the elemental mechanisms of action and advise evidence-based practice.
Patient’s perspective
At the beginning of the treatment, the patient was advised that a full recovery from her injury was not possible, so no positive outcomes were expected one year after the injury. But little is known about the effects of EA for neurological injuries, and the scientific literature reinforces the idea that after one year of a SCI no improvements are expected.
The patient expressed her gratitude for the improvements obtained, and regained hope which allowed her to quit her antidepressant medication. At the moment, the patient continues ongoing electroacupuncture sessions and strongly believes she will recover her ability to walk.
Acknowledgments
The authors would like to thank the patient for participating in this study as well as Universitat Internacional de Catalunya (UIC).
Funding: None.
Footnote
Reporting Checklist: The authors have completed the CARE reporting checklist. Available at https://lcm.amegroups.com/article/view/10.21037/lcm-21-69/rc
Peer Review File: Available at https://lcm.amegroups.com/article/view/10.21037/lcm-21-69/prf
Conflicts of Interest: All authors have completed the ICMJE uniform disclosure form (available at https://lcm.amegroups.com/article/view/10.21037/lcm-21-69/coif). The authors have no conflicts of interest to declare.
Ethical Statement: The authors are accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. All procedures performed in this study were in accordance with the ethical standards of the institutional and/or national research committee(s) and with the Helsinki Declaration (as revised in 2013). Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the editorial office of this journal.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Shavelle RM, DeVivo MJ, Brooks JC, et al. Improvements in long-term survival after spinal cord injury? Arch Phys Med Rehabil 2015;96:645-51. [Crossref] [PubMed]
- Hagen EM. Acute complications of spinal cord injuries. World J Orthop 2015;6:17-23. [Crossref] [PubMed]
- Hicken BL, Putzke JD, Richards JS. Bladder management and quality of life after spinal cord injury. Am J Phys Med Rehabil 2001;80:916-22. [Crossref] [PubMed]
- Thygesen MM, Jønsson AB, Rasmussen MM, et al. Characteristics in a traumatic spinal cord injury population. Dan Med J 2020;67:A09190490. [PubMed]
- La Rosa G, Conti A, Cardali S, et al. Does early decompression improve neurological outcome of spinal cord injured patients? Appraisal of the literature using a meta-analytical approach. Spinal Cord 2004;42:503-12. [Crossref] [PubMed]
- van Middendorp JJ, Hosman AJ, Doi SA. The effects of the timing of spinal surgery after traumatic spinal cord injury: a systematic review and meta-analysis. J Neurotrauma 2013;30:1781-94. [Crossref] [PubMed]
- Fan Q, Cavus O, Xiong L, et al. Spinal Cord Injury: How Could Acupuncture Help? J Acupunct Meridian Stud 2018;11:124-32. [Crossref] [PubMed]
- Chen YY, Zhang W, Chen YL, et al. Electro-acupuncture improves survival and migration of transplanted neural stem cells in injured spinal cord in rats. Acupunct Electrother Res 2008;33:19-31. [Crossref] [PubMed]
- Hao CZ, Wu F, Guo Y, et al. Acupuncture for neurogenic bladder after spinal cord injury: a systematic review and meta-analysis. Eur J Integr Med 2013;5:100-8. [Crossref]
- Lewith G, Vincent C. Evaluation of the clinical effects of acupuncture. Pain Forum 1995;4:29-39.
- White AR, Filshie J, Cummings TM, et al. Clinical trials of acupuncture: consensus recommendations for optimal treatment, sham controls and blinding. Complement Ther Med 2001;9:237-45. [Crossref] [PubMed]
- Lei H, Fu Y, Xu G, et al. Different types of acupuncture and moxibustion therapy for neurogenic bladder after spinal cord injury: A systematic review and network meta-analysis study protocol. Medicine (Baltimore) 2020;99:e18558. [Crossref] [PubMed]
- Zhang T, Liu H, Liu Z, et al. Acupuncture for neurogenic bladder due to spinal cord injury: a systematic review protocol. BMJ Open 2014;4:e006249. [Crossref] [PubMed]
- Shen Y, Zhang F, Xu Y, et al. Myofascial trigger point electroacupuncture for perineal pain: a case report. Acupunct Med 2021;39:396-7. [Crossref] [PubMed]
- Cuthbert SC, Goodheart GJ Jr. On the reliability and validity of manual muscle testing: a literature review. Chiropr Osteopat 2007;15:4. [Crossref] [PubMed]
- Wang YZ, Yang JX, Wang JX. Electroacupuncture for ileus following laparoscopic radical cystectomy and Bricker urinary diversion: a case report. Acupunct Med 2021;39:545-6. [Crossref] [PubMed]
- Kim YJ. Acupuncture management of blepharoptosis: a case report. Acupunct Med 2020;38:201-2. [Crossref] [PubMed]
- Yoon SH, Baek JH, Leem J. Improved grip myotonia in a patient with myotonic dystrophy type 1 following electroacupuncture therapy: A CARE-compliant case report. Medicine (Baltimore) 2020;99:e21845. [Crossref] [PubMed]
- Wen Q, Li N, Wang X, et al. Effect of electroacupuncture versus solifenacin for moderate and severe overactive bladder: a multi-centre, randomized controlled trial study protocol. BMC Complement Med Ther 2020;20:224. [Crossref] [PubMed]
- Dorsher PT, McIntosh PM. Acupuncture's Effects in Treating the Sequelae of Acute and Chronic Spinal Cord Injuries: A Review of Allopathic and Traditional Chinese Medicine Literature. Evid Based Complement Alternat Med 2011;2011:428108. [Crossref] [PubMed]
Cite this article as: Alcoba Kait J, Estivill E, Cabanas-Valdés R. Effectiveness of electroacupuncture for a patient with a complete traumatic spinal cord injury: a case report. Longhua Chin Med 2022;5:19.