
The anatomic, clinical, and physiologic correspondences of myofascial trigger points and classical acupuncture points
Introduction
Chronic musculoskeletal pain conditions are consistently among the top reasons patients seek advice and treatment from health care providers (1,2). Musculoskeletal pain afflicts 85% of the population at some point during their lives (3); and myofascial pain syndrome (MPS) is the most common musculoskeletal pain condition, having a global prevalence of 14–47% (4). MPS prevalence increases with age, afflicting 37–65% of individuals ages 30–60 (5,6), and 85% of those over age 65 (7). In 2019, the United Nations reported that globally, the percentage of individuals ≥65 years of age had increased from 6% to 9% of the total population over the prior three decades, with that percentage predicted to rise to 16% by 2050 (8). Chronic musculoskeletal pain (including MPS) not only may cause physical disability and impair the quality of life for afflicted individuals, but also creates significant economic burdens on national health care systems. The economic impact of chronic pain in the United States in 2010 was estimated to be 635 billion dollars, with pain treatment costs representing approximately half that total (9). Musculoskeletal pain was determined to be the second leading health expenditure in Canada (10).
Though there were intermittent reports published by European physicians regarding muscle pain disorders as early as the mid-1500’s, systematic studies of mTrPs and their referred-pain patterns largely occurred in the 20th century, with the term “myofascial trigger point” first introduced by Travell and Rinzler in 1952 (11). Travell and Simons were the first authors to fully compile the existing MPS literature (including their 4+ decades of MPS research) into a reference textbook- the 1st edition of the Trigger Point Manual, which was published in 2 separate volumes in 1983 and 1992 (12,13). This reference illustrates 255 “most common” mTrP locations (all but 2 in muscles), their clinical uses, and their myofascial referred-pain patterns. All mTrPs can produce spontaneous pain, and ~25% of these mTrPs also have associated non-pain clinical effects described including tinnitus, chronic cough, and belching/vomiting (12). In the 30 years since the initial release of the Trigger Point Manual, the subsequent two editions of this reference text have only added data for 5 new mTrP locations (14).
The allopathic medicine standard for treating MPS is outlined in the Trigger Point Manual, which includes mTrP deactivation with injections, stretches, exercise, nutrition, medications, and ergonomic/lifestyle modifications. Though early MPS practitioners typically treated/deactivated mTrPs via injections using local anesthetic with or without corticosteroid, the Trigger Point Manual documents mTrPs can also be deactivated by dry needling (12). Within the past 2 decades In the United States, there has been marked expansion of myofascial pain dry needling skill certification from 1 state to 36 states for physical therapists, who utilize acupuncture needles to deactivate mTrPs via dry needling in MPS patient treatments (15,16). Two states now are also allowing occupational therapist certification for dry needling (16).
Musculoskeletal and in particular MPS have afflicted humans throughout history, and mTrPs likely are not modern discoveries, as the Huangdi Neijing in the 27th article described similar clinical findings 2,200 years ago: “The pains of multitude impediment occur at fixed places… at times they appear and at times they rest… the wind cold and dampness settle in the flesh and compress the flesh, making the fluids coagulate to become froth. The froth is affected by cold and condenses. The condensation extrudes the textures of the muscles to make them split. The splitting causes pain and the pain makes the blood converge. The convergence of the blood produces heat (inflammation)….” (17).
Practitioners versed in both the acupuncture and MPS traditions will sense their clinical and physiologic similarities, though acupuncture and trigger points are described using vastly different terminologies, and the two traditions utilize different approaches to needling their points (12,13,17-19).
There has been controversy since the 1970’s regarding whether any anatomic, clinical and/or physiologic relationship exists between these “most common” mTrPs described by Travell and Simons (and other MPS researchers) and the classical acupuncture points and primary channels described by Traditional Chinese Medicine millennia previously (20-28). If those mTrPs and classical acupoints can be shown to be similar anatomically, clinically, and/or physiologically, this not only would allow integration of ancient and contemporary clinical and research databases to optimally treat MPS and other non-pain conditions, but also would have potential importance in elucidating acupuncture’s mechanisms.
The purpose of this review is to summarize prior literature findings regarding the anatomic, clinical, and physiologic correspondences of the “most common” mTrPs illustrated by Travell and Simons in the 1st edition of the Trigger Point Manual and classical acupuncture points, and the clinical implications of these relationships.
History of trigger point to acupuncture point comparisons
The first attempt to formally compare the MPS and acupuncture traditions was performed nearly 50 years ago by Melzack et al. in their 1977 Journal of Pain article, which concluded a 71% concordance between mTrPs and acupuncture points in the treatment of pain disorders exists (22). That study examined mTrP locations in thorax as described by three prior research studies (Table 1) and compared them to acupuncture points in terms of anatomic locations and pain indications (22,29,30,32). There was partial overlap of the mTrP locations described in those three studies examined, so only 48 discrete mTrP locations and their pain indications remained to compare to those of acupuncture points.
Melzack et al.’s study found 100% anatomic correspondence of these 48 mTrP locations to acupuncture point locations, but the clinical correspondences in treating pain of these anatomically corresponding trigger-acupuncture point pairs varied from 64% to 100% (Table 1) in the 3 studies examined (22). The overall 71% correspondence of trigger and acupuncture points in treating pain disorders led its authors to postulate that these points represent the same phenomenon, possibly explained by their having common underlying neural mechanisms (22).
Melzack et al.’s study’s limitations included that only 48 discrete mTrPs were examined, and its criteria for correlating acupuncture points to these trigger points was conceptionally questionable (22). The study arbitrarily defined the mTrP and acupoint locations it examined as anatomically corresponding if the points were located within 3 cm of each other—no attempt was made to determine if the correlated acupuncture points even entered the muscle of its anatomically corresponding trigger point.
A quarter century later, Birch reviewed the data and findings of that 1977 study, reaching a nearly opposite conclusion—that at most there was an 18–19% correspondence of the trigger and acupuncture points examined in Melzack et al.’s study, and that conceptually these mTrPs should have been correlated only to the ashi class of acupoints (23). Birch opined that of the acupoints examined in that 1977 study, 61% were “not recommended at all” and only 19% were “commonly recommended” for the treatment of pain disorders, and that 44% of those acupoints were “not recommended for anything” according to the acupuncture references utilized in his analysis (23). Both the Shanghai College of Tradition Medicine and Deadman acupuncture references, however, document that all but 2 classical acupoints (BL-8 and ST-17) do have pain indications described, which reflect hundreds to thousands of years of accumulated clinical knowledge and experience (18,19).
The Birch study was incomplete- despite having had availability to another 200+ “most common” mTrPs’ data described in the Trigger Point Manual, the Birch study only examined 48 mTrPs for their potential correlation to acupoints (12,13,23). Birch also opined that mTrPs should only be compared to ashi points, as ashi points are the only acupoint type defined by the presence of tenderness (like mTrPs). This is a conceptually flawed conclusion, as authoritative acupuncture references and research studies document that when a viscera or musculoskeletal area is clinically involved, relevant acupuncture points characteristically do become tender (19,31,33-36). As examples, classical or “extra” acupoints may be exquisitely tender when clinically involved—a patient with lateral epicondylitis may point to the location of LI-10 or LI-11 as their ashi (“that’s it) tender point, or patients with sciatica may point to the location of BL-54 as their ashi point. The Spiritual Axis itself in Chapter 51 states “…when they (acupuncture points) are pressed, there should be pain and a sunken sensation.” (37). Thus, the acupuncture theorists who assert that classical acupoints should not be correlated to mTrPs but rather only to ashi points are conceptually incorrect, and their view is contradicted by multiple authoritative acupuncture references and scientific studies (23,28,38).
The only systematic comparison of the complete MPS trigger point database as delineated in the 1st edition of the Trigger Point Manual to classical acupoints was published in a 3-part series in 2008–2009 by Dorsher and Fleckenstein (12,13,25-27). This database was developed in 2006 comparing all 255 of the “most common” mTrPs illustrated in the 1st edition of the Trigger Point Manual to classical acupoints, including their anatomic locations, their clinical (pain and non-pain) indications, and their physiologic relationships (myofascial referred-pain to primary channel distributions). This database was validated at the University of Munich by Dr. Dominik Irnich’s research group in 2006–2007 (25) using multiple authoritative anatomic, MPS, and acupuncture references (12,13,18,19,39-41). Eachou Chen’s cross-sectional acupuncture point anatomy atlas (42) provided additional, definitive confirmation that any anatomically proximate “most common” trigger point and classical acupuncture point pairs found in this analysis influence the same muscles (or muscle regions).
This 2006 database found that for the 255 “most common” mTrPs in 135 muscles illustrated in the 1st edition of the Trigger Point Manual, there was an anatomically corresponding classical acupuncture point in >93% (238/255) of instances (25). “Anatomically corresponding” was defined as being present when a classical acupoint location was anatomically proximate to a “most common” mTrP illustrated location and entered the same muscle region of that mTrP (12,13,25).
Of those 238 anatomically corresponding trigger-acupuncture point pairs found in the study, 221 (94%) had similar regional pain indications described by the Trigger Point Manual and acupuncture references (12,13,18,19,26). The statistical odds that this could occur by chance is infinitesimally small (~1/2221).
The Trigger Point Manual describes non-pain (somatovisceral) effects for 60 (24%) of the 255 “most common” mTrPs illustrated therein, including tinnitus, chronic cough, and dizziness (12,13). The 2006 database documents that those 60 mTrPs’ somatovisceral effects were similar to those described for their “anatomically corresponding” classical acupoints in 56/60 (93%) instances (26). The statistical odds that this could occur by chance is infinitesimally small (~1/256).
The 2006 database also examined the relationships of mTrP myofascial referred-pain distributions illustrated in the Trigger Point Manual to those of the primary channels for each of the 238 anatomically corresponding “most common” trigger point- acupuncture point pairs found (12,13,27). 17 of those mTrPs (“cardiac arrhythmia”, “belch button”, and “causes diarrhea” mTrPs) have no referred-pain patterns described by the Trigger Point Manual (12). Of the remaining 221 anatomically corresponding trigger-acupuncture point pairs, 201 (91%) demonstrated correspondences (overlaps) of their referred-pain and primary channel distributions (12,13,27). Again, the statistical odds that their distributions would overlap by chance is infinitesimally small (~1/2201).
Overall, the 2006 mTrP-acupoint database evidences that the “most common” mTrPs illustrated in the 1st edition of the Trigger Point Manual have fundamental similarities to classical acupoints in terms of their anatomic locations, clinical (pain and non-pain) indications, and physiologic (referred-pain to Channel distribution) properties, confirming the conclusions of Melzack et al.’s 1977 study (22,25-27). The 2006 database’s findings of marked (>90%) clinical and physiologic correspondences of “anatomically corresponding” trigger-acupuncture point pairs furthers that their anatomic correspondences are extremely unlikely to represent chance findings (<1/256 ≤1 in 7 trillion odds statistically).
The limitations of these three studies based on the 2006 trigger-acupuncture point database include that the results are correlational, though the “most common” mTrP and classical acupoint location comparisons were independently validated and extensive anatomic verification using authoritative anatomic atlases and acupuncture anatomy references. Also, the 2006 database used the acupuncture references of Deadman and the Shanghai College of Traditional Medicine to determine classical acupuncture point pain and non-pain indications, which differed from the acupuncture references used by Melzack et al.’s and Birch’s studies (18,19,22,23).
Discussion
Melzack et al.’s 1977 study (22) opined that acupuncture points and Channels are conceptual and without scientific evidence, as opposed to trigger points that are “grounded in science”. In reality, there has never been a proven pathoanatomic basis for trigger points (22,43). While ultrasound elastography may be helpful to identify mTrP areas, to date there is no “gold standard” objective method (i.e., pathology, imaging) to definitively identify mTrPs (44).
The 255 “most common” mTrP locations illustrated in the 1st edition of the Trigger Point Manual along with their pain/non-pain indications and myofascial referred-pain patterns reflect the most frequent and arguably the most clinically important mTrP locations, based on Travell and Simons’ 4+ decades of clinical experience/research and their synthesis of prior MPS literature cited within that reference (12,13). These “most common” mTrP locations were never meant to be considered the only mTrP locations in the body, as explicitly stated by those authors in the first volume of the Trigger Point Manual (12). There have been only 5 additional “common” mTrP locations with illustrated referred-pain patterns added in subsequent editions of the Trigger Point Manual, despite the publication of >17,000 scientific papers regarding MPS since the initial publication of the Trigger Point Manual 40 years ago (14,45). This suggests that there have been few other “common” mTrP locations subsequently found in this extensive MPS literature base.
Some researchers have implied that in contrast to the well-described classical acupoint locations, mTrPs are not well localized (18,19,23). The locations of “common” mTrP locations as described by Travell and Simons are illustrated with “X”’s in specific muscle locations (12,13). Other early MPS researchers also illustrated focal muscle areas where they located “trigger zones” in their studies, not the more general muscle localizations shown in the 3rd (latest) edition of the Trigger Point Manual (14,29,30,32) (Figure 1).

Thus, the “most common” mTrP locations as illustrated by Travell and Simons in the 1st edition of the Trigger Point Manual not only are well localized, but also are the only mTrPs with specific referred-pain patterns and clinical indications (including non-pain uses) described (12,13).
Analogous to the 255 “most common” trigger points, the 361 classical acupoints are not the only acupuncture points described. The Shanghai College of Medicine acupuncture reference describes hundreds of other acupoints including the “miscellaneous” and “new” points, which are mostly non-channel in location, as well as the ashi class of acupoints (18). The classical acupoints can be conceptualized as being the most commonly used and/or clinically important acupuncture points, based on hundreds to thousands of years of clinical practice observations by countless acupuncturists. Recall that 349/361 (95%) of the classical acupoints were described by 282 CE in the Systematic Classic of Acupuncture and Moxibustion, including 49 midline acupoints (18).
As previously outlined, authoritative acupuncture references as well as the Spiritual Axis itself document the importance of finding the presence of classical acupoint tenderness for points associated with injury/illness (19,35-37). Contemporary research studies confirm sensitization of acupuncture points associated with injury/illness (18,31,33,34).
Thus, there is a plausible conceptual basis for comparing the “most common” mTrPs and classical acupoints both in terms of their anatomic locations, clinical indications, and physiologic properties.
The marked difference between the pain treatment correspondences calculated for the same 48 trigger-acupuncture point pairs examined in both the Melzack et al. and Birch studies (71% vs. 18–19%, respectively) might partly be explained by the differing acupuncture references each study used (22,23). More likely, the difference is related to the methodology Birch utilized—i.e., determining whether the multiple acupuncture references “commonly recommended” the correlated acupuncture points for treating pain or not (23). That study’s report that 61% of the correlated acupoints are “not recommended at all for the treatment of pain” is implausible, as both the Shanghai College of Traditional Medicine and Deadman acupuncture references document that all but 2 classical acupuncture points (BL-8 and ST-17) do have pain indications described (18,19). These acupuncture point pain indications reflect hundreds to thousands of years of accumulated clinical knowledge and experience of countless acupuncturists. Whether or not the pain indication of a given classical acupoint is “commonly recommended” or not is irrelevant- that pain indication exists and should have been used for the correlation analysis. In fact, all 35 acupuncture points correlated to mTrPs in Melzack et al.’s study do have pain indications described by these two acupuncture references, so these acupoints’ pain indications correlated to those of mTrPs in 31/35 (89%) of comparisons (18,19,22). This result is comparable to the 94% pain indication correspondences of the “most common” mTrPs and classical acupoints found by Dorsher and Fleckenstein’s study (26). Further, the overwhelming (93%) clinical correspondences of these anatomically corresponding trigger-acupuncture point pairs in treating non-pain conditions found by the 2006 database provides further evidence of the clinical/physiologic similarities of these points (26).
The >90% correspondences found of the myofascial referred-pain and Primary channel distributions of these anatomically corresponding trigger-acupoint pairs provides additional physiologic evidence of these point pairs’ fundamental similarities (27). These findings not only provide independent physiologic evidence that generating myofascial referred-pain during dry needling of mTrPs and the spread of needle sensation (qi) during acupuncture needle stimulation likely are describing the same physiologic phenomenon, but also that this mTrP referred-pain data can be used to provide physiologic validation of primary channel theory, as shown in Figure 2 (46).
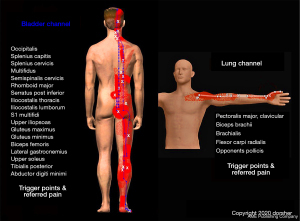
Figure 2 demonstrates that the “most common” mTrPs that anatomically correspond to Bladder (BL) classical acupoints in the 2006 database have referred-pain distributions that follow the Bladder channel distribution, and when summed together serve to replicate the course of the Bladder channel from the frontal region of the head all the way down to the fifth toe (25,27,46). Similarly, mTrPs that anatomically correspond to Lung (LU) classical acupoints have referred-pain distributions along the anterior chest and anterolateral upper extremity in a Lung channel distribution, and when summed together serve to replicate the course of the Lung channel from the anterior chest down the arm to the thumb (25,27,46). Other examples of how myofascial referred-pain distributions can be used to validate other Primary channels are available in the medical literature (46). These findings provide even further physiologic evidence that the similarities of the referred-pain and channel distributions for anatomically corresponding trigger-acupuncture point pairs found in the 2006 database are not chance findings (27).
The Dorsher and Fleckenstein (25,26) and Melzack et al. (22) studies both found strong correspondences of common trigger points and acupuncture points anatomically (93–100%) and in the treatment of pain (71–94%) (22,25,26). Both studies came to similar conclusions regarding the potential anatomic/physiologic mechanisms for these correspondences: “trigger points and acupuncture points for pain, though discovered independently and labeled differently, represent the same phenomenon and can be explained in terms of the same underlying neural mechanisms” (22). A plausible anatomic and physiologic basis for these pain indication similarities as well as other clinical and physiologic similarities has been offered previously, as shown in Figure 3 (27).
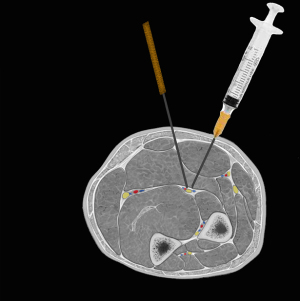
Figure 3 demonstrates that whether an acupuncture needle is inserted between bone, tendon, or muscles to reach the “true” location of a classical acupoint, or whether a myofascial pain specialist inserts a needle into/through a muscle belly to reach a “most common” mTrP location and invoke a “twitch response”, the needle tips likely meet at the neurovascular bundles coursing through the intermuscular layers of the body or at motor end plate of muscles near the needle tips (12). Then the “twitch response” can be readily explained to be a fasciculation of muscle fibers innervated by the nerve (or motor endplate) that is mechanically depolarized by the needle tips (47-50). There has been recent anatomic evidence published demonstrating the close anatomic relationship of the “most common” mTrP locations to cranial and peripheral nerve branches where they enter the abductor hallucis, gluteus maximus, and trapezius muscles (51,52). This is consistent with Simons et al.’s findings that motor endplate noise is significantly more prevalent at trigger point locations than in sites outside of a trigger point location but within the motor endplate zone: “endplate noise seems to be characteristic of, but is not restricted to, the region of a myofascial trigger point” (53). Those findings have been confirmed independently by Couppé et al. and Ge et al. (54,55).
Conclusions
The 255 “most common” trigger points illustrated in the 1st edition of the Trigger Point Manual are fundamentally similar to classical acupuncture points anatomically, clinically (pain and non-pain indications), and physiologically (myofascial referred-pain to primary channel distributions). These mTrPs’ referred-pain distributions can even be utilized to reproduce the distributions of the primary channels, thus serving to validate channel theory. These multiple correspondences of these trigger and acupuncture points strongly evidence that they are likely describing the same clinical phenomenon, as Melzack et al. had suggested 45 years ago, and are probably united by common underlying neurologic mechanisms. These 255 “most common” trigger points illustrated in the 1st edition of the Trigger Point Manual can be then viewed as a partial contemporary rediscovery of the anatomic and clinical findings of the acupuncture tradition thousands of years before, though with differing “languages” and needling techniques.
Myofascial pain practitioners can benefit by the 2,000+ years of accumulated clinical experience and knowledge contained in the acupuncture tradition database. Conversely, acupuncturists can benefit by the clinical research, scientific techniques, and data outlined by the MPS database. Integration of these ancient and contemporary clinical and research databases together could serve to optimize the treatment of MPS as well as other non-pain conditions and have importance in elucidating myofascial pain’s and acupuncture’s anatomic and/or physiologic mechanisms, with common neurologic mechanisms likely uniting both traditions. Finally, this reviews’ findings may have important implications regarding appropriate educational standards for dry needling training and certification statutes.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at https://lcm.amegroups.com/article/view/10.21037/lcm-21-47/coif). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- St Sauver JL, Warner DO, Yawn BP, et al. Why patients visit their doctors: assessing the most prevalent conditions in a defined American population. Mayo Clin Proc 2013;88:56-67. [Crossref] [PubMed]
- Finley CR, Chan DS, Garrison S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician 2018;64:832-40. [PubMed]
- Staud R. Future perspectives: pathogenesis of chronic muscle pain. Best Pract Res Clin Rheumatol 2007;21:581-96. [Crossref] [PubMed]
- Wada JT, Akamatsu F, Hojaij F, et al. An Anatomical Basis for the Myofascial Trigger Points of the Abductor Hallucis Muscle. Biomed Res Int 2020;2020:9240581. [Crossref] [PubMed]
- Jonsson E, Nachemson A. Collected knowledge about back pain and neck pain. What we know–and what we don’t know. Lakartidningen 2000;97:4974-80. [PubMed]
- Drewes AM, Jennum P. Epidemiology of myofascial pain, low back pain, morning stiffness and sleep-related complaints in the general population. J Musculoskelet Pain 1995;3:121.
- Podichetty VK, Mazanec DJ, Biscup RS. Chronic non-malignant musculoskeletal pain in older adults: clinical issues and opioid intervention. Postgrad Med J 2003;79:627-33. [Crossref] [PubMed]
- United Nations, Department of Economic and Social Affairs, Population Division (2019). World Population Ageing 2019: Highlights (ST/ESA/SER.A/430).
- Gaskin DJ, Richard P. The economic costs of pain in the United States. J Pain 2012;13:715-24. [Crossref] [PubMed]
- Health Canada: Economic Burden of Illness in Canada. Ottawa: Health Canada; 1998. Available online: https://publications.gc.ca/site/archivee-archived.html?url=https://publications.gc.ca/collections/Collection/H21-136-1998E.pdf
- Shah JP, Thaker N, Heimur J, et al. Myofascial Trigger Points Then and Now: A Historical and Scientific Perspective. PM R 2015;7:746-61. [Crossref] [PubMed]
- Travell JG, Simons DG. Myofascial pain & dysfunction: The Trigger Point Manual. Vol. 1. Baltimore: Williams & Wilkins, 1983.
- Travell JG, Simons DG. Myofascial pain and dysfunction: The Trigger Point Manual. Vol. 2, The lower extremities. Baltimore: Williams & Wilkins, 1992: 607.
- Donnelly JM, editor. Travell, Simons & Simons’ myofascial pain and dysfunction: The Trigger Point Manual. 3rd edition. Philadelphia, PA: Wolters Kluwer, 2019:968.
- American Physical Therapy Association. State laws and regulations governing dry needling performed by physical therapists in the U.S. 2020. Available online: https://www.apta.org/contentassets/eef3804fb78c4c3a81e38b23e5ce5b01/apta_dry_needling_laws_by_state.pdf
- Myopain Seminars. Available online: https://www.myopainseminars.com/about-us/. Accessed 10/12/2021
- Ming Z, translator. The Medical Classic of The Yellow Emperor. Beijing: Foreign Languages Press, 2001:304.
- O’Connor J, Bensky D, editors. Acupuncture: a comprehensive text. O’Connor J, Bensky D, translators. Chicago: Eastland Press, 1981:741.
- Deadman P, Al-Khafaji M, Baker K. A manual of acupuncture. Hove, East Sussex (England): Journal of Chinese Medicine Publications, 1998:667.
- Peng ZF, Nan GE, Cheng MN, et al. The comparison of trigger point acupuncture and traditional acupuncture. Zhongguo Zhen Jiu 2008;28:349-52. [PubMed]
- Hong CZ. Myofascial trigger points: pathophysiology and correlation with acupuncture points. Acupunct Med 2000;18:41-7. [Crossref]
- Melzack R, Stillwell DM, Fox EJ. Trigger points and acupuncture points for pain: correlations and implications. Pain 1977;3:3-23. [Crossref] [PubMed]
- Birch S. Trigger point--acupuncture point correlations revisited. J Altern Complement Med 2003;9:91-103. [Crossref] [PubMed]
- Huang QM, Xu AL, Ji LJ, et al. Understanding of myofascial trigger points (2): acupuncture vs dry needling. Phys Med Rehabil Int 2018;5:1146.
- Dorsher PT, Fleckenstein J. Trigger points and Classical acupuncture points: Part 1: Qualitative and quantitative anatomic correspondences. Deutsche Zeitschrift für Akupunktur 2008;51:15-24. [Crossref]
- Dorsher PT, Fleckenstein J. Trigger points and Classical acupuncture points: Part 2: Clinical correspondences in treating pain and somatovisceral disorders. Deutsche Zeitschrift für Akupunktur 2008;51:6-11. [Crossref]
- Dorsher PT, Fleckenstein J. Trigger points and acupuncture points. Part 3: Relationships of myofascial referred pain patterns to acupuncture meridians. Deutsche Zeitschrift fur Akupunktur 2009;52:6-11.
- Jiang S, Zhao JS. The historical source of “trigger points”: classical ASHI points. World Journal of Acupuncture Moxibustion 2016;26:11-4. [Crossref]
- Sola AE, Kuitert JH. Myofascial trigger point pain in the neck and shoulder girdle. Northwest Med 1955;54:980-4. [PubMed]
- Kennard MA, Haugen FP. The relationship of subcutaneous focal sensitivity to referred pain of cardiac origin. Anesthesiology 1955;16:297-311. [Crossref] [PubMed]
- Li F, He T, Xu Q, et al. What is the acupoint? A preliminary review of acupoints. Pain Medicine 2015;16:1905-15. [Crossref] [PubMed]
- Rinzler SH, Travell J. Therapy directed at the somatic component of cardiac pain. Am Heart J 1948;35:248-68. [Crossref] [PubMed]
- Chen S, Miao Y, Nan Y, et al. The study of dynamic characteristic of acupoints based on the primary dysmenorrhea patients with the tenderness reflection on Diji (SP 8). ECAM 2015. Available online:
10.1155/2015/158012 10.1155/2015/158012 - Tan H, Tumilty S, Chapple C, et al. Understanding acupoint sensitization: a narrative review on phenomena, potential mechanism, and clinical application. ECAM 2019. Available online:
10.1155/2019/6064358 10.1155/2019/6064358 - Wiseman N, Ellis A. Fundamentals of Chinese Medicine. Brookline: Paradigm Publishers, 1996:124.
- Helms JM. Acupuncture Energetics: A Clinical Approach for Physicians. Berkeley (CA): Medical Acupuncture Publishers, 1995:246.
- Spiritual Axis, Chapter 51. Circa 200 BCE. O’Connor J, Bensky D, translators. Chicago: Eastland Press, 1981:103.
- Chen D, Yang G, Wang F, et al. Discussing the relationship among the ASHI point, tender point and myofascial trigger point. Zhongguo Zhen Jiu 2017;37:212-4. [PubMed]
- Gray H. Anatomy of the Human Body. Available online: https://www.bartleby.com/107/. accessed 10/12/2021.
- Clemente CD. Anatomy: a regional atlas of the human body. 2nd ed. Baltimore: Urban & Schwarzenberg, 1981.
- Netter FH. Atlas of human anatomy. Summit: Ciba-Geigy, 1989.
- Chen E. Cross-sectional anatomy of acupoints. Edinburgh: Churchill Livingstone, 1995:244.
- Quintner JL, Bove GM, Cohen ML. A critical evaluation of the trigger point phenomenon. Rheumatology (Oxford) 2015;54:392-9. [Crossref] [PubMed]
- Do TP, Heldarskard GF, Kolding LT, et al. Myofascial trigger points in migraine and tension-type headache. J Headache Pain 2018;19:84. [Crossref] [PubMed]
- PubMed literature search engine. Available online: https://pubmed.ncbi.nlm.nih.gov/. Accessed 10/26/2021.
- Dorsher PT. Myofascial referred-pain data provide physiologic evidence of acupuncture meridians. J Pain 2009;10:723-31. [Crossref] [PubMed]
- Julian FJ, Goldman DE. The effects of mechanical stimulation on some electrical properties of axons. J Gen Physiol 1962;46:297-313. [Crossref] [PubMed]
- Meadows JC. Observations on the responses of muscle to mechanical and electrical stimuli. J Neurol Neurosurg Psychiatry 1971;34:57-67. [Crossref] [PubMed]
- Matsuura S. Depolarization of sensory nerve endings and impulse initiation in common carotid baroreceptor. J Physiol 1973;235:31-56. [Crossref] [PubMed]
- Hogan QH. Pathophysiology of peripheral nerve injury during regional anesthesia. Reg Anesth Pain Med 2008;33:435-41. [Crossref] [PubMed]
- Akamatsu FE, Yendo TM, Rhode C, et al. Anatomical basis of the myofascial trigger points of the gluteus maximus muscle. Biomed Res Int 2017;2017:4821968. [Crossref] [PubMed]
- Akamatsu FE, Ayres BR, Saleh SO, et al. Trigger points: an anatomical substratum. Biomed Res Int 2015;2015:623287. [Crossref] [PubMed]
- Simons DG, Hong CZ, Simons LS. Endplate potentials are common to midfiber myofacial trigger points. Am J Phys Med Rehabil 2002;81:212-22. [Crossref] [PubMed]
- Couppé C, Midttun A, Hilden J, et al. Spontaneous needle electromyographic activity in myofascial trigger points in the infraspinatus muscle: a blinded assessment. J Musculoskel Pain 2001. Available online:
10.1300/J094v09n03_02 10.1300/J094v09n03_02 - Ge HY, Fernández-de-Las-Peñas C, Yue SW. Myofascial trigger points: spontaneous electrical activity and its consequences for pain induction and propagation. Chin Med 2011;6:13. [Crossref] [PubMed]
Cite this article as: Dorsher PT. The anatomic, clinical, and physiologic correspondences of myofascial trigger points and classical acupuncture points. Longhua Chin Med 2022;5:7.

