Gut flora “the second brain” connects Eastern and Western medicine: intestinal hyper-permeability or Qi deficiency can affect brain, mind, and whole body
2,000 years ago, Hippocrates (the “Father of modern medicine”) and Traditional Chinese Medicine doctors were probably thinking the same thing. Gut microbiota imbalance (dysbiosis) can be a root cause of brain/mind/physical disorders which are related to “Qi energy” deficiency
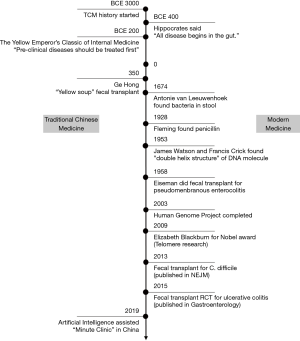
“All disease begins in the gut.” (Hippocrates, a Greek physician who lived around 400 BCE) (Figure 1) “You are what you eat.” (Anthelme Brillat-Savarin, a French lawyer and politician wrote in his book in 1826) “You have a second brain in your gut.” (modern scientists’ quote) “I have a gut feeling.” (people would feel like this when they are nervous.)
There are number of interesting phrases and quotes regarding the “Brain-Mind-Gut axis” even 2,000 years ago in the modern medicine world. As a matter of fact, this had been already addressed by Traditional Chinese Medicine (TCM) doctors since 3000 BCE (about 5,000 years ago). For example, “The Yellow Emperor’s Classic of Internal Medicine (Huangdi Neijing)” is the first textbook which was compiled and edited around 200 BC (Figure 1), and the Yin-Yang theory and Qi energy have been the core essence of TCM. Especially, the abdomen (for instance CV4 acupuncture point “Guanyuan” located 2 inches below the umbilicus) has been considered as one of the most important parts to generate Qi which is “vital energy” to nourish whole body (internal organs, brain, heart, skin, muscle, and mind). This is why diet and herbal therapy are vital to human lives according in the TCM world. Interestingly, “fecal transplantation” was first documented in a TCM textbook around CE 350—a Chinese physician, Ge Hong treated acute food poisoning patients by a therapy called “yellow soup” which was made from a healthy person’s stool (Figure 1).
On the other hand, about 2,000 years after Hippocrates passed away, science based modern medicine has advanced very rapidly. In 1674, Antonie van Leeuwenhoek, a Dutch scientist first found bacteria in the stool. In 1928, Sir Alexander Fleming, a Scottish physician found penicillin, and the progress of modern medicine has been accelerated rapidly. Although antibiotics saved millions of people’s lives from infectious diseases, the overuse triggered different issues such as antibiotics-resistant bacteria and pseudomembranous enterocolitis (PE). In 1958, Dr. Ben Eiseman, an American surgeon treated PE patients by fecal transplantation (Figure 1) (1). This was about 1,600 years later than Ge Hong did the fecal transplantation in China, and he probably thought that this should improve the patients’ Qi production. This is one of the most beautiful examples to understand what were in common between TCM and modern science.
As genome sequencing technique advanced dramatically in the 21st century, scientists have found that the number of total microbiota (“gut flora”) per person could be 100 trillion (2) while the number of normal cells of one human body is about 60 trillion. In addition, total microbial genes are over 3.3 million which outnumbers human genes by 150:1 which gives us the sense of “second brain in the gut” and “Brain-Mind-Gut axis.” For instance, short-chain fatty acid (SCFA) which is produced inside the colon when the bacteria ferments fibers is considered to be beneficial to prevent diseases in multiple organs such as colon cancer (3), liver cancer (4), obesity, and diabetes (5). SCFA can also send signals to the brain in order to suppress appetite and modulate systemic immune system (6). With further scientific advancement, in 2013, a randomized clinical trial of fecal microbiota transplantation (FMT) revealed significant effectiveness for refractory Clostridium difficile infection (7). Now there is no doubt that gut microbiota imbalance which is called “dysbiosis” is strongly related to “Qi deficiency.”
Dysbiosis triggers “Intestinal hyper-permeability” (modern science) which is almost same as “Qi deficiency” (TCM). “Bad things” in the gut could be spread systemically to affect whole body, brain, and mind—systemic inflammation, immune imbalance, and multi-organ dysfunction
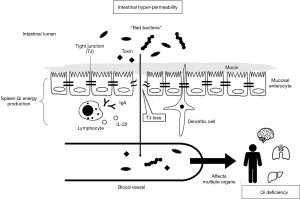
In recent years, a non-technical term “Leaky gut” has been used frequently by healthcare bloggers. Professionally, this is referred as “intestinal hyper-permeability” (Figure 2). When dysbiosis happens inside the intestinal lumen, “bad things” (such as pathogenic bacteria and toxin) start passing through the intestinal wall and go into the bloodstream (“leaking” from the intestinal lumen to outside of the intestine), and consequently be spread to the whole body to affect multiple organs.
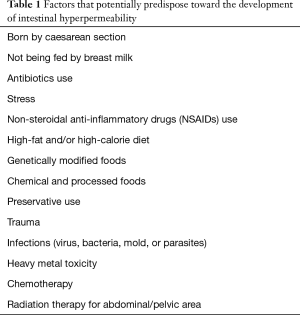
There is an “intestinal mucosal barrier” [this term was first adopted by Cummings (8) in 2004] where bidirectional interaction (“cross talk”) happen all the time between “non-self antigens” (such as microorganisms, toxins, and foods) and normal cells (such as enterocytes and immune cells including dendritic cells) (9). Normally, this “cross talk” regulates molecular trafficking (via interleukin-22, Immunoglobulin A, and so forth) and the intestine acquire tolerance or immunity to “outsiders.” However, when this barrier is damaged (loss of tight junction between mucosal enterocytes) due to some reasons (Figure 2 and Table 1), “bad things” start passing through the barrier which is the state of “intestinal hyper-permeability.” This could consequently cause chain reactions involving multiple organs leading to systemic inflammation, immune imbalance, and oxidative stress (10). According to TCM theory, “Qi deficiency” triggers multi-organ dysfunction and there are a lot in common with “intestinal hyper-permeability.” Therefore, it would be very reasonable to say that “intestinal hyper-permeability” and “Qi deficiency” are very similar or almost same pathopysiology.
Full table
A prescription to heal a country? How can we stop the healthcare crisis which is associated with exponential rise in the cost? Let’s borrow ancient wisdom from TCM preventive medicine, and treat “pre-clinical disease” by taking care of the gut (regarding intestinal permeability and Qi energy)
What is “pre-clinical disease” in TCM? In “Huangdi Neijing (The Yellow Emperor’s Classic of Internal Medicine),” there is a sentence “Great physicians do not treat disease, but they treat pre-clinical disease.” (Figure 1) In another classical TCM textbook “Qian Jin Fang”, it is described that “Top level physicians heal the whole country, middle level physicians treat people, while lower level physicians treat diseases only.” This means that the top level physicians can save the country by treating “pre-clinical disease.”
“Pre-clinical disease” is the state with some symptoms but (almost) no abnormalities in the tests [for instance, irritable bowel syndrome (IBS), chronic fatigue, migraine, or cold sensitivity], or the state with no symptoms but some test abnormalities (for instance, metabolic syndrome and obesity). Scientifically, microbiota dysbiosis is related to advanced glycation end-products (AGEs) which are glycated proteins/lipids as a result of exposure to sugars. AGEs damage blood vessels’ endothelial function by suppressing nitric oxide and producing inflammatory cytokines (11), and consequently trigger arteriosclerosis (“arterial aging”) (12), and metabolic syndrome. Sir William Osler [1849–1919], a Canadian physician who is also described as the “Father of Modern Medicine” (so is Hippocrates) said “A man is as old as his arteries.” Qi deficiency, dysbiosis, intestinal hyper-permeability, and pre-clinical diseases—these are all related to each other (13,14), and there is no doubt that some natural interventions based on TCM should be applied as the first step of preventive medicine. Borrowing ancient wisdom might save many countries from their healthcare cost crisis.
If patients have chronic symptoms involving three or more different organs, intestinal hyper-permeability and Qi deficiency should be strongly suspected
Factors that potentially predispose toward the development of intestinal hyper-permeability (Figure 2) include being born by Caesarean section, not being fed by breast milk, frequent antibiotics use, stress, non-steroidal anti-inflammatory drugs (NSAIDs) use, high-fat and/or high-calorie diet, genetically modified foods, chemical or processed foods, preservative use, trauma, infections (virus, bacteria, mold, or parasites), and heavy metal toxicity (Table 1). If a patient presents with chronic symptoms involving three or more organs, for instance, fatigue, bloating, and frequent colds, Qi deficiency should be strongly suspected (Figure 3). Once serious conditions [such as cancers, liver/kidney failure, hypothyroidism, inflammatory bowel diseases (IBDs), or brain diseases] are ruled out by tests (blood test, X-ray, CT/MRI, or endoscopy as needed), the TCM-based diagnosis of Qi deficiency can be made. Other common symptoms of Qi deficiency include insomnia, constipation/diarrhea, abdominal pain, cold hands/feet, migraine/tension headache, sinus congestion, dry skin, hair loss, chemical sensitivity, smell sensitivity, and so forth. Especially, cold hands/feet is a very important finding in the TCM diagnostic system, and the severe one is considered as Raynaud’s syndrome (fingers and toes turn white/blue and feel cold and numb). From modern medicine standpoint, the cause of Raynaud’s attack is still unknown, but this is one of the typical signs of Qi deficiency in TCM.
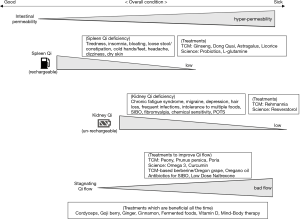
Two different “Qi” are important from the standpoint of intestinal permeability. Spleen Qi is related to food, and Kidney Qi is related to telomere. Kidney Qi deficiency would cause stronger symptoms than Spleen Qi deficiency
As each person has different DNA, each person has different microbiota (“microbial fingerprints”) (15), which means the TCM diagnosis and treatment would be different from person to person. In TCM, there are five different Qi energies (five element theory) with different treatments, but two of them, Spleen and Kidney Qi are especially related to intestinal function. (Please note: “Spleen” or “Kidney” in TCM are different from the real organs of spleen and kidney.) (Figure 3).
Roughly speaking, “Spleen Qi” is made from food-related nutrients absorbed by the digestive system. Therefore, harmful foods triggers microbial dysbiosis, and this leads to impaired production of Spleen Qi. While Spleen Qi is also called “acquired Qi” which people can creat by themselves after they are born, “Kidney Qi” is also called “inherited Qi” which people inherit from their parents, and its amount is highest at birth but decreases by aging. Kidney Qi seems to be directly related to genetic makeup, especially “telomere” which is a region of repetitive DNA sequences at the end of a chromosome, and protects the end of the chromosome from deterioration. Its length is longest at birth, but it becomes shorter by aging (15,000 at birth, but will decrease to 8,000 around age 35). Its importance has been deeply researched by Dr. Elizabeth Blackburn who was awarded for Nobel prize in 2009 (Figure 1). If telomere becomes shorter, the chromosome becomes unstable. This state disturbs the cell to divide, and consequently increases overall health risks, impairs multiple organs, and leads to premature mortality (16-20). In addition, psychological stress can also shorten telomere (21-23). This is why telomere and Kidney Qi seem to be strongly and directly related.
In order to understand TCM concept easier, please imagine a motor vehicle equipped with “hybrid energy” which are gasoline and (un-rechargeable) battery. They correspond to Spleen and Kidney Qi respectively (Figure 3). Gasoline can be fueled repetitively (Spleen Qi can be increased again by eating beneficial foods), but the battery (Kidney Qi) is difficult to be recharged. However, if microbial dysbiosis happens, Spleen Qi level decreases (“out of gas”) and people presents multiple symptoms at the same time including tiredness, insomnia, bloating, loose stool/constipation, cold hands/feet, headache, dizziness, or dry skin. If this remains unhealed, Kidney Qi (“electric power”) starts to be consumed and intestinal permeability becomes very high. People’s symptoms become intense, long-lasting, and complicated, such as chronic fatigue syndrome, migraine, depression, hair loss, frequent infections, intolerance to multiple foods, small intestinal bacterial overgrowth (SIBO), fibromyalgia, chemical sensitivity, or postural orthodontic tachycardia syndrome (POTS).
“Stagnating flow” can happen with Qi deficiency. This state might be related to autoimmune disorders or “Rheuma”-tic diseases (Note: In Greek, “Rheuma” means “flow.”)
“Stagnating flow” is a unique diagnosis in TCM system (Figure 3). Qi is supposed to flow smoothly throughout the body all the time, but when the amount of Qi decreases (Qi deficiency), the flow becomes less smooth. Some symptoms and conditions such as menstrual disorder, hemorrhoids, joint pain, some autoimmune disorders including Hashimoto’s thyroiditis are partially related to Stagnating flow. General rheumatic (autoimmune) disorders are also related to this state. In Chinese, rheumatic disorders are written as “Wind and Humid.” In TCM, “wind” would irritate the skin which is a “barrier/defense mechanism” from outsiders, and scientifically this “wind issue” means immune system imbalance since there are many immune cells such as Langerhans cells in human’s skin. “Humid issue” refers to whole body congestion due to “stagnating Qi flow” which leads to multiple joint inflammation.
On the other hand, interestingly, about 500 years after Hippocrates passed away, ancient Greek doctors (Hippocrates’ followers) analyzed joint disorders by using words “Rrheo” or “Rheuma” whose meaning was “flow.” They had an idea that “something good” were flowing from brain to whole body inside healthy human’s bodies all the time, but joint inflammation/swelling could happen due to “flow disturbance.” Science and TCM had already had something in common even 1500 years ago.
Treatment for Spleen Qi deficiency. Ginseng, Astragalus, Dong Quai, Licorice, Ginger, Jujube, and Cinnamon are beneficial. Probiotics and L-glutamine are useful to repair and rebuild the gut. TCM + modern science = Synergetic effect
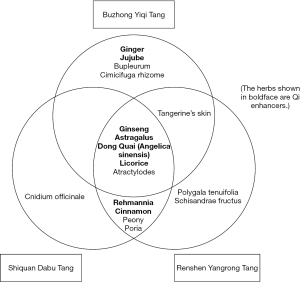
Most of TCM remedies are blend of multiple herbs and natural things, and there are three frequently-used herbal remedies to increase (Spleen) Qi based on 5,000-year experience—Buzhong Yiqi Tang, Shiquan Dabu Tang, and Renshen Yangrong Tang (Figure 4). Especially, Ginseng, Astragalus, Dong Quai (Angelica sinensis), and Licorice are used in all three remedies, and they are considered as “herbal Qi energy booster” or adaptogen. Most of these herbs have been already studied scientifically. For instance, Ginseng is also called “Panax” in Greek which means “all-healing” since scientists thought Ginseng was beneficial for variety of diseases. Astragalus has anti-fatigue effect (24,25). Licorice has some data regarding the benefit or repairing gastric damage and to relieve stress (26,27) which exactly means restorative effect for Spleen Qi in the TCM theory. Dong Quai is often described in Western IM as a good estrogenic herb for menopausal women, but its essence is that Dong Quai is effective to increase Qi for both women and men for all ages. In addition, some of those remedies contain ginger, jujube (dates), and cinnamon (Figure 4) which are also consumed as healthy snacks or cooking spice. They are also considered to be “Qi-increasing foods.”
From modern medicine side, probiotics and L-glutamine are used in Western IM since they are specifically good to “rebuild or strengthen” the gut system (Figure 3). Today variety of over-the-counter supplement type probiotics (“good bacteria”) are available worldwide, and this should be beneficial to increase Spleen Qi. L-glutamine is an amino acid which is helpful to repair damages in the intestinal lining (28). This is rich in bone broth, grass-fed beef, asparagus, turkey, and so forth.
Treatment for Kidney Qi deficiency. Rehmannia is a good TCM herb. Resveratrol might be a good Western IM treatment
In TCM world, Liuwei Dihuang Wan which is a blend of six (“Liu” means six) different herbs, is one of effective remedies to increase Kidney Qi. Among the six herbs, the most important one is Rehmannia (“Dihuang” in Chinese) (Figure 3) which is beneficial for immune system (29), gut microbiota, and obesity (30).
From modern science side, resveratrol (Figure 3) might be good to restore telomere (31) which should be beneficial to increase Kidney Qi. This is rich in red wine, skin of grapes/blueberries/raspberries/peanuts, and also available as over-the-counter supplements in many countries. Studies (21-23,32) also showed that meditation and positive psychological change was associated with higher levels of telomerase activity. This explains the connection among Kidney Qi, telomere, and mind-body medicine.
Other Qi-enhancing (for both Spleen and Kidney Qi) TCM therapy
Cordyceps (“Dongchong Xiacao” in Chinese) which is a fungus that lives on certain caterpillars is also very effective to enhance energy, immune system, male sexual function and so forth by increasing both Spleen and Kidney Qi (especially Kidney) (Figure 3). It also has scientific data showing the benefit for microbiota and intestinal immunity (33,34). Goji berry (“Gouqi” in Chinese) has multiple beneficial effects including immune and energy enhancement, anti-oxidant, anti-inflammation, and improving hypertension/hyperlipidemia/diabetes.
Treatment for “Stagnating flow.”
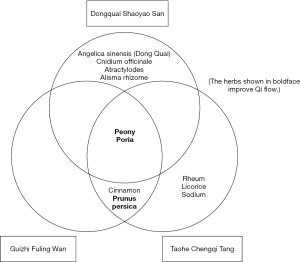
There are three major blended remedies to make the energy flow smoother. Donquai Shaoyao San, Guizhi Fuling Wan, Taohe Chengqi Tang (Figure 5). Peony (“Shaoyao” in Chinese), Prunus persica (“Taoren”), and Poria (“Fuling”) are used in those remedies, and these are considered to be anti-inflammatory herbs, roughly speaking. From modern science side, Omega 3-rich oils (made from fish or flaxseed) or Curcumin are frequently used as natural anti-inflammatory medications (Figure 3) (35,36).
Fungal (yeast) dysbiosis—yeast syndrome?
Fungal (yeast) dysbiosis is a controversial topic, and there is little evidence to support that “gut yeast syndrome” could cause fatigue, headache, bloating, and poor memory. It is considered normal to find yeast in the gut, but an overgrowth of yeast may exacerbate existing inflammatory bowel disease (IBD) such as ulcerative colitis or Crohn’s disease (37,38). Some doctors believe anti-fungal pharmaceutical medications are beneficial for this “yeast syndrome,” but there are no clinical trials that document the efficacy, and these medications should not be used due to strong concern of creating drug-resistant yeast.
However, if some patients who have developed acute candida (fungal) vaginitis with medical history of chronic fatigue and IBS take an anti-fungal medication which has been officially prescribed to treat vaginitis (not for intestinal dysbiosis), their abdominal symptoms and fatigue may also improve unexpectedly. This could be just a coincidence or a placebo effect, but there is a hypothesis that reducing candida has resulted in good bacteria increase in the gut. If this phenomenon is analyzed by TCM’s “Yin and Yang” theory, that would mean just “removing a burden” can promote human’s own “self-healing ability” without fueling any energy.
For this purpose, berberine which is one of benzylisoquinoline alkaloids found in plants is useful as a “natural antibiotic” to reduce yeast in the gut. Berberine has been used in TCM as Phellodendron amurense (PA, “Huangbo”) or Coptic chinensis (CC, “Huanglian”), and is widely available as over-the-counter supplements such as Oregon grape in the U.S. and Europe (Figure 3). In Western Integrative Medicine (IM) area, oregano oil is a different botanical products which can be used for the same purpose (39,40), and this is also available as an over-the-counter supplement.
Small intestinal bacterial overgrowth (SIBO) is another factor of microbiota dysbiosis. There are specific diagnostic tests and useful antibiotics. Qi-enhancing herbs might be of value to reduce SIBO recurrence
Unlike fungal dysbiosis, SIBO which is a state that “bad bacteria” have grown abnormally has a definitive diagnostic criterion using breath tests (Glucose/Fructose/Lactulose). The mainstay of therapy is oral antibiotics such as rifaximin, metronidazole, and neomycin to reduce bacteria, and approximately 60 percent of patients respond to the treatment while rest of them have persistent symptoms or frequent recurrence (41). Some patients have underlying issues (diabetes-related abnormal intestinal motility, alcoholism, cirrhosis, or excessive proton pump inhibitor use) while some do not. Since probiotics are not adequate to prevent SIBO recurrence (42) in many cases, adding TCM herbs might be useful. The “berberine containing herbs” (PA and CC) and oregano oil can reduce bad bacteria, and “Qi-increasing herbs” (Ginseng, Astragalus, Dong Quai, Licorice, Rehmannia, Cordyceps, and Goji berry) can grow good bacteria faster (Figure 3). Combining pharmaceutical medications for (sub)acute problems and TCM for prevention or chronic maintenance seems to be a very reasonable way, but further research is warranted.
Low dose naltrexone (LDN) therapy has anti-inflammatory effect (scientific standpoint) or Qi flow-improving effect (TCM standpoint)
This new therapy is to use naltrexone, a medication for opioid or alcohol dependence, at very low dosage (only about 5% of usual dosage). Clinical reports of LDN have demonstrated possible benefits in multiple sclerosis, fibromyalgia, cancers (lung and kidney) (43,44), Crohn’s disease, or psoriasis by reducing systemic inflammation. Our clinical impression is that LDN’s effect is similar to Donquai Shaoyao San (DSS) which is one of commonly used herbal remedies to correct “Stagnating Qi flow” although these two are completely different treatments. Especially, “Yin type” people who have “sensitive stomach” and the whole body being “slightly thin” tend to experience more benefit from LDN or DSS.
For instance, for those who have just ran full marathon (42.195 km or 26.2 miles) and are completely exhausted, they cannot run any more even if they were given some “energy drink.” Instead, if they receive “gentle leg massage” therapy, they might able to run another mile. In some cases, improving Qi flow “smoother” is more effective rather than giving Qi energy. This seems to be how LDN and DSS works in a similar way, but scientific research (e.g., if DSS reduces LDN-related inflammation markers) is definitely warranted.
Diet therapy
Diet is as critical as herbal therapy, and it consists of two parts, which are removing “bad foods” and increasing “good foods.” For Qi deficiency, reducing refined sugar, dairy products, and gluten is reasonable to try since those foods have higher likelihood of triggering dysbiosis-related intestinal and systemic inflammation. In the U.S., number of patients would experience remarkable improvement by reducing gluten for digestive issues, fatigue, pain, or mood even if they were proved not to have Celiac disease. It is strongly suspected that microbial dysbiosis and gluten sensitivity are partially related to each other.
“Good foods” include probiotic-rich fermented foods, such as Douchi (fermented soy beans) and Furu (fermented Tofu), and “Qi-increasing foods” such as ginger, bone broth, cinnamon, black pepper, dates (jujube), tangerine’s skin.
Benefit of vitamin D
Vitamin D is important for gut health and Qi since it can influence the composition of gut microbiota (45) and decrease inflammation in the gut (46,47). If serum level is low, supplementing Vitamin D seems to be effective to improve Spleen/Kidney Qi deficiency and stagnating flow from TCM standpoint (Figure 3).
Mind-body therapy is beneficial to increase Spleen/Kidney Qi
As described above, some researches suggest that psychological stress can also shorten telomere (21-23), and this might be related to reduction in Kidney Qi. As shown in Table 1, stress can increase the intestinal permeability, and this will probably lead to Spleen Qi reduction. Considering this Brain-Mind-Gut connection, mind-body therapy should be useful for both Spleen and Kidney Qi deficiency (Figure 3).
Cancer treatment and Qi deficiency
Since the cell division speed of the digestive tract cells is generally faster than other organs cells, those who undergo chemotherapy and/or radiation therapy for abdominal/pelvic area tend to experience treatment-related digestive adverse effects (Table 1) more frequently. Needless to say, main stream of cancer treatment must be conventional therapies (surgery, medications, and radiation), but from standpoint of the gut, their adverse effects are considered as “accidentally created” intestinal hyper-permeability or Qi deficiency. Even after these treatments are completed, many cancer survivors would have chronic aftereffects such as fatigue, IBS, immunosuppression (frequent infection), or neuropathy. Treatments to improve intestinal permeability and Qi energy should be beneficial for these chronic symptoms. Particularly, Ginseng has been already well studied in some randomized double-blinded clinical trials, and it is considered to be useful for chronic fatigue for cancer survivors (48,49).
Basically, TCM herbal remedies should not be administered for those who under active chemotherapy or molecularly targeted therapy due to the concern for unfavorable drug-to-herb interactions. Those who are under active treatment or has a treatment history with immune check point inhibitors such as anti-PD1/PDL1/CTLA4 antibodies should avoid TCM herbs, probably indefinitely. These drugs are remarkably effective for certain cancers (such as melanoma, non-small cell lung cancer, and renal cell carcinoma), but it is reported that anti-cancer immune effect may last for decades (or maybe forever) in some patients even if they have already completed the immune check point inhibitors therapy. Since Qi-enhancing herbs could boost up patients’ immune system, “too much immune enhancement” may occur even 5 or 10 years after the immune check point inhibitors therapy is finished.
A suggestion for the new era of IM: computer technology can combine modern science, Western IM, and TCM into one?
Artificial intelligence (AI) has “deep learning” technology which has been inspired by information processing in human brains, and it has been revolving rapidly since 2010. AI is already used in some medical fields such as genetic diagnosis to medical charts’ voice recognition, and it can also interpret radiology scans 150 times faster than humans. It would be safe to say “today AI has come of age.” Since the gut microbiota “second brain” is an extremely complicated system (much smarter than the “real brain”), AI which is by far more functional than human brain will be used more frequently in the future for the microbiota researches, stool tests, and gut flora treatments. On the other hand, in China, AI-assisted, TCM-style history taking computer and portable wrist pulse diagnostic device are about to be utilized at number of “minute clinics” in 2019. According to some TCM experts, they are able to “predict” and obtain “80% impression” of diagnosis only by history taking. Rest of it (20%) can be obtained by adding physical exams such as pulse diagnosis, tongue exam, and face expression reading. As a matter of fact, these exams sometimes could be more useful than history taking when making a diagnosis and determining the treatment plan. However, these experts strongly believe that the time for physical exams is critical to “establish rapport” with patients since touching (human to human) is the most beautiful and valuable communication tool in the medical field.
“Prediction” and “humanity” are the masterpieces of ancient traditional medicine, and they are exactly what are needed in the clinical settings today. In the future, AI should be used more both in TCM (diagnosis and treatment) and stool microbiota test, and this will make it easier for doctors to find “pre-clinical diseases” before they become “real diseases.” In addition, AI can do “daunting tasks” on behalf of human doctors, and this will help healthcare providers to spend more time with patients, and to prevent providers’ burnout and depression. The overarching goal is to bring back the humanity since the medical provider-patient relationship is a founding principle of health care. These masterpieces of TCM can be integrated into modern medicine by making the most of computer technology.
Another masterpiece is the fact that 5 to 10 different herbs/natural things are blended to create one remedy in TCM. The blending is expected to create “synergetic effect” (e.g., 1+1+1 becomes 10 or 20) but its mechanism has been very difficult to understand by Western IM practitioners. There has been a very big wall between TCM and Western IM for many years, and unfortunately, it still exists at this present time. However, there is a possibility that AI might be able to remove the wall by making the TCM’s “theory of synergetic blending of multiple herbs” understandable to Western IM doctors. Even if it remains non-understandable, AI can assist TCM beginners to create the best personalized natural remedies.
On the other hand, one of the biggest advantages of science is the visualization of the diagnostic process and the treatment effectiveness. As human nature, since we are surrounded by computer technology all the time today, we tend to prefer seeing the evidence of diagnosis and treatment visually, especially in numbers. For instance, even if the Clostridium difficile infection is cured by the fecal transplantation therapy and the patients are feeling much better for their digestive system, they may also want to know how the number of “key bacteria” such as bacteroidetes or firmicutes have changed before/after the transplantation. Even if TCM herbal therapy could significantly improve the symptoms of autonomic dysfunction for instance, patients may say “please test my pulse pattern with the machine so that I can see the treatment effectiveness in number.” In the past, patients were totally satisfied when TCM treatments just improved their symptoms. But today, patients may not feel in the same way, or they want something more. This difference between science and TCM seems to have been giving Western IM doctors the feeling of “they are two different languages.” For this purpose, AI may be able to change TCM diagnosis and treatment process to numeric information which is understandable to everyone.
Conclusions
“You can obtain novel insight by studying old wisdom.” This is one of sentences in The Analects (“Lunyu” in Chinese) which is a collection of Chinese sayings, traditionally believed to have been compiled around 300 BCE. Even 2,500 years ago, philosophers respected the ancient wisdom. For many years, it has been relatively challenging to understand TCM from scientific point of view, but genome analysis technology (such as DNA sequencing) and microbiota researches have enabled us to understand the strong relationship between TCM and modern medicine.
As mentioned above, about 2,000 years ago, Chinese physicians said “top level physicians can save the country by treating pre-clinical diseases” which should be started from treatments to improve gut microbiota balance and heal intestinal hyper-permeability or Qi deficiency. Constant demand for wellbeing, unmet needs for whole person care, mind-body connection, patient-centeredness, a new paradigm in primary and preventive health care, cost-conscience treatment, and personalized plan—all of these must be practiced by healthcare providers right now since many countries are facing healthcare financial crisis which unfortunately, is expected to continue getting worse. Integration of ancient wisdom, modern science, and AI seems to be one of the best solution for this issue. It is strongly anticipated that AI’s deep learning technology would greatly accelerate the process of “connecting dots” in the fields of TCM and modern science to “make lines or shapes.”
If a patient has a diagnosed disease, for instance Rheumatoid arthritis, modern medicine’s guideline-based therapy such as methotrexate should be considered first. If a patient’s medical issue is migraine only, serotonin 5-hydroxytryptamine (5-HT) receptor agonists (“Triptans”) or some TCM herbal remedies which contain Evodia (“Wu zhu yu” in Chinese) might be most effective. However, in today’s modern society, increasing number of people present to clinics with “pre-clinical disease” which is associated with multiple symptoms, but without a definitive diagnosis. For instance, some patients have been struggling with chronic headache, fatigue, depressive mood, and eczema at the same time, but unfortunately they would feel “lost” since they do not know which specialist to see (or they have to see all of the specialists?).
We should first consider some interventions to heal the “root causes” which are often related to the gut microbiota imbalance and Qi deficiency since “you are what you eat.” The treatment should be “tailor-made” since everyone has different level of stress, different symptoms, different DNA, and different microbiota (so-called “microbial fingerprints”). Even for fecal transplantation which is a “cutting-edge” treatment, it is known that the treatment effectiveness would vary due to the difference in DNA of each patient’s normal cells.
What I described in this article is just a rough sketch for Brain-Mind-Gut connection, or it could be only hypothesis-raising. Therefore, more scientific research is warranted for TCM to be utilized and well accepted in the new era of IM. Number of TCM herbs have been already researched scientifically (for instance, Ginseng for energy, Astragalus for immune system, and Licorice for digestion) with promising results. However, rather than assessing each herb separately, we should move to the next phase which is to elucidate the real essence of synergetic effects of multi-herbal TCM remedies with possible help from AI. AI-assisted TCM research combined with genome-analysis precision medicine will become the best pathway for the future of preventive medicine.
Acknowledgments
Funding: None.
Footnote
Conflicts of Interest: The author has completed the ICMJE uniform disclosure form (available at http://dx.doi.org/10.21037/lcm.2019.04.01). The author has no conflicts of interest to declare.
Ethical Statement: The author is accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Open Access Statement: This is an Open Access article distributed in accordance with the Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License (CC BY-NC-ND 4.0), which permits the non-commercial replication and distribution of the article with the strict proviso that no changes or edits are made and the original work is properly cited (including links to both the formal publication through the relevant DOI and the license). See: https://creativecommons.org/licenses/by-nc-nd/4.0/.
References
- Eiseman B, Silen W, Bascom GS, et al. Fecal enema as an adjunct in the treatment of pseudomembranous enterocolitis. Surgery 1958;44:854-9. [PubMed]
- Qin J, Li R, Raes J, et al. A human gut microbial gene catalogue established by metagenomic sequencing. Nature 2010;464:59-65. [Crossref] [PubMed]
- McNabney SM, Henagan TM. Short chain fatty acids in the colon and peripheral tissues: a focus on butyrate, colon cancer, obesity, and insulin resistance. Nutrients 2017;9:1348. [Crossref] [PubMed]
- Bindels LB, Porporato P, Dewulf EM, et al. Gut microbiota-derived propionate reduces cancer cell proliferation in the liver. Br J Cancer 2012;107:1337-44. [Crossref] [PubMed]
- Yadav H, Lee JH. Beneficial metabolic effects of a probiotic via butyrate-induced GLP-1 hormone secretion. J Biol Chem 2013;288:25088-97. [Crossref] [PubMed]
- Furusawa Y, Obata Y, Fukuda S, et al. Commensal microbe-derived butyrate induces the differentiation of colonic regulatory T cells. Nature 2013;504:446-50. [Crossref] [PubMed]
- van Nood E, Vrieze A, Nieuwdorp M, et al. Duodenal infusion of donor feces for recurrent Clostridium difficile. N Engl J Med 2013;368:407-15. [Crossref] [PubMed]
- Cummings JH, Antoine JM, Azpiroz F, et al. PASSCLAIM--gut health and immunity. Eur J Nutr 2004;43:II118-II173. [Crossref] [PubMed]
- Kamada N, Chen GY, Inohara N, et al. Control of pathogens and pathobionts by the gut microbiota. Nat Immunol 2013;14:685-90. [Crossref] [PubMed]
- Bischoff SC, Barbara G, Burrman W, et al. Intestinal permeability-a new target for disease prevention and therapy. BMC Gastroenterol 2014;14:189. [Crossref] [PubMed]
- Thornalley PJ. Dietary AGEs and ALEs and risk to human by their interaction with the receptor for advanced glycation endproducts (RAGE)-an introduction. Mol Nutr Food Res 2007;51:1107-10. [Crossref] [PubMed]
- Baynes JW, Thorpe SR. Glycoxidation and lipoxidation in atherogenesis. Free Radic Biol Med 2000;28:1708-16. [Crossref] [PubMed]
- Wang Z, Klipfell E, Bennett BJ, et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 2011;472:57-63. [Crossref] [PubMed]
- Vich Vila A, Imhann F, Collij V, et al. Gut microbiota composition and functional changes in inflammatory bowel disease and irritable bowel syndrome. Sci Transl Med 2018; [Crossref] [PubMed]
- Franzosa EA, Huang K, Meadow JF, et al. Identifying personal microbiomes using metagenomic codes. Proc Natl Acad Sci U S A 2015;112:E2930-8. [Crossref] [PubMed]
- Epel ES, Lin J, Wilhelm FH, et al. Cell aging in relation to stress arousal and cardiovascular disease risk factors. Psychoneuroendocrinology 2006;31:277-87. [Crossref] [PubMed]
- Ornish D, Lin J, Daubenmier J, et al. Increased telomerase activity and comprehensive lifestyle changes: a pilot study. Lancet Oncol 2008;9:1048-57. [Crossref] [PubMed]
- Njajou OT, Hsueh WC, Blackburn EH, et al. Association between telomere length, specific causes of death, and years of healthy life in health, aging, and body composition, a population-based cohort study. J Gerontol A Biol Sci Med Sci 2009;64:860-4. [Crossref] [PubMed]
- Farzaneh-Far R, Lin J, Epel E, et al. Telomere length trajectory and its determinants in persons with coronary artery disease: longitudinal findings from the heart and soul study. PLoS One 2010;5:e8612 [Crossref] [PubMed]
- Farzaneh-Far R, Lin J, Epel ES, et al. Association of marine omega-3 fatty acid levels with telomeric aging in patients with coronary heart disease. JAMA 2010;303:250-7. [Crossref] [PubMed]
- Epel ES, Blackburn EH, Lin J, et al. Accelerated telomere shortening in response to life stress. Proc Natl Acad Sci U S A 2004;101:17312-5. [Crossref] [PubMed]
- Puterman E, Lin J, Blackburn E, et al. The power of exercise: buffering the effect of chronic stress on telomere length. PLoS One 2010;5:e10837 [Crossref] [PubMed]
- Jacobs TL, Epel ES, Lin J, et al. Intensive meditation training, immune cell telomerase activity, and psychological mediators. Psychoneuroendocrinology 2011;36:664-81. [Crossref] [PubMed]
- Liu CH, Tsai CH, Li TC, et al. Effects of the traditional Chinese herb astragalus membranaceus in patients with poststroke fatigue: a double-blind, randomized, controlled preliminary study. J Ethnopharmacol 2016;194:954-62. [Crossref] [PubMed]
- Zhang G, Zhou SM, Zheng SJ, et al. Astragalus on the anti-fatigue effect in hypoxic mice. Int J Clin Exp Med 2015;8:14030-5. [PubMed]
- Dehpour AR, Zolfaghari ME, Samadian T, et al. The protective effect of liquorice components and their derivatives against gastric ulcer induced by aspirin in rats. J Pharm Pharmacol 1994;46:148-9. [Crossref] [PubMed]
- Methlie P, Husebye EE, Hustad S, et al. Grapefruit juice and licorice increase cortisol availability in patients with Addison's disease. Eur J Endocrinol 2011;165:761-9. [Crossref] [PubMed]
- van der Hulst RR, van Kreel BK, von Meyenfeldt MF, et al. Glutamine and the preservation of gut integrity. Lancet 1993;341:1363-5. [Crossref] [PubMed]
- Xu L, Zhang W, Zeng L, et al. Rehmannia glutinosa polysaccharide induced an anti-cancer effect by activating natural killer cells. Int J Biol Macromol 2017;105:680-5. [Crossref] [PubMed]
- Han K, Bose S, Kim YM, et al. Rehmannia glutinosa reduced waist circumferences of Korean obese women possibly through modulation of gut microbiota. Food Funct 2015;6:2684-92. [Crossref] [PubMed]
- Latorre E, Birar VC, Sheerin AN, et al. Small molecule modulation of splicing factor expression is associated with rescue from cellular senescence. BMC Cell Biol 2017;18:31. [Crossref] [PubMed]
- Lavretsky H, Epel ES, Siddarth P, et al. A pilot study of yogic meditation for family dementia caregivers with depressive symptoms: effects on mental health, cognition, and telomerase activity. Int J Geriatr Psychiatry 2013;28:57-65. [Crossref] [PubMed]
- An Y, Li Y, Wang X, et al. Cordycepin reduces weight through regulating gut microbiota in high-fat diet-induced obese rats. Lipids Health Dis 2018;17:276. [Crossref] [PubMed]
- Fan ST, Nie SP, Huang XJ, et al. Protective properties of combined fungal polysaccharides from Cordyceps sinensis and Ganoderma atrum on colon immune dysfunction. Int J Biol Macromol 2018;114:1049-55. [Crossref] [PubMed]
- Calder PC. Omega-3 fatty acids and inflammatory processes: from molecules to man. Biochem Soc Trans 2017;45:1105-15. [Crossref] [PubMed]
- He Y, Yue Y, Zheng X, et al. Curcumin, inflammation, and chronic diseases: how are they linked? Molecules 2015;20:9183-213. [Crossref] [PubMed]
- Sokol H, Leducq V, Aschard H, et al. Fungal microbiota dysbiosis in IBD. Gut 2017;66:1039-48. [Crossref] [PubMed]
- Böhringer M, Pohlers S, Schulze S, et al. Candida albicans infection leads to barrier breakdown and a MAPK/NF-κB mediated stress response in the intestinal epithelial cell line C2BBe1. Cell Microbiol 2016;18:889-904. [Crossref] [PubMed]
- Sakkas H, Papadopoulou C. Antimicrobial activity of basil, oregano, and thyme essential oils. J Microbiol Biotechnol 2017;27:429-38. [Crossref] [PubMed]
- Leyva-López N, Gutiérrez-Grijalva EP, Vazquez-Olivo G, et al. Essential oils of oregano: biological activity beyond their antimicrobial properties. Molecules 2017; [Crossref] [PubMed]
- Lauritano EC, Gabrielli M, Scarpellini E, et al. Small intestinal bacterial overgrowth recurrence after antibiotic therapy. Am J Gastroenterol 2008;103:2031-5. [Crossref] [PubMed]
- Zhong C, Qu C, Wang B, et al. Probiotics for preventing and treating small intestinal bacterial overgrowth: a meta-analysis and systematic review of current evidence. J Clin Gastroenterol 2017;51:300-11. [Crossref] [PubMed]
- Toljan K, Vrooman B. Low-dose naltrexone (LDN) - review of therapeutic utilization. Med Sci (Basel) 2018; [Crossref] [PubMed]
- Miskoff JA, Chaudhri M. Low dose naltrexone and lung cancer: a case report and discussion. Cureus 2018;10:e2924 [PubMed]
- Waterhouse M, Hope B, Krause L, et al. Vitamin D and the gut microbiome: a systematic review of in vivo studies. Eur J Nutr 2018; [Epub ahead of print]. [Crossref] [PubMed]
- Raftery T, O’Morain CA, O’Sullivan M. Vitamin D: new roles and therapeutic potential in inflammatory bowel disease. Curr Drug Metab 2012;13:1294-302. [Crossref] [PubMed]
- Tabatabaeizadeh SA, Tafazoli N, Ferns GA, et al. Vitamin D, the gut microbiome and inflammatory bowel disease. J Res Med Sci 2018;23:75. [Crossref] [PubMed]
- Barton DL, Soori GS, Bauer BA, et al. Pilot study of Panax quinquefolius (American ginseng) to improve cancer-related fatigue: a randomized, double-blind, dose-finding evaluation: NCCTG trial N03CA. Support Care Cancer 2010;18:179-87. [Crossref] [PubMed]
- Barton DL, Liu H, Dakhil SR, et al. Wisconsin ginseng (Panax quinquefolius) to improve cancer-related fatigue: a randomized, double-blind trial, N07C2. J Natl Cancer Inst 2013;105:1230-8. [Crossref] [PubMed]
Cite this article as: Umeda N. Gut flora “the second brain” connects Eastern and Western medicine: intestinal hyper-permeability or Qi deficiency can affect brain, mind, and whole body. Longhua Chin Med 2019;2:6.